NCM 102 Study Guide
1. Ethico-Moral and Legal Foundations of Client Education
1.1 Ethical Principles in Education
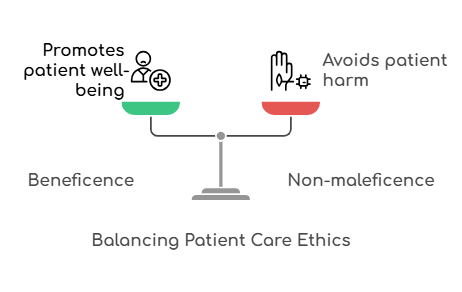
1.1.1 Beneficence and Non-maleficence
-
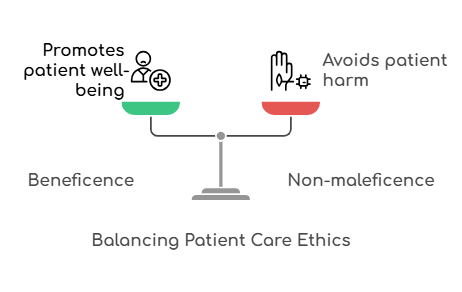
Beneficence refers to the ethical obligation to act for the
benefit of the patient, promoting their well-being and health.
-
Non-maleficence emphasizes the duty to avoid causing harm
to patients.
-
Together, these principles guide nurses in making decisions that prioritize
patient welfare while minimizing risks.
1.1.2 Justice and Fairness
-
Justice in healthcare education means ensuring that all
patients have equal access to education and resources, regardless of their
background.
-
Fairness involves treating all patients with impartiality
and respect, ensuring that no one is disadvantaged.
-
These principles are crucial for fostering trust and equity in the
nurse-patient relationship.
1.1.3 Respect for Autonomy
-
Autonomy is the right of patients to make informed
decisions about their own healthcare.
-
Nurses must respect patients’ choices and provide them with the necessary
information to make those choices.
- This principle reinforces the importance of patient-centered care.

1.2 Legal Considerations in Health Education
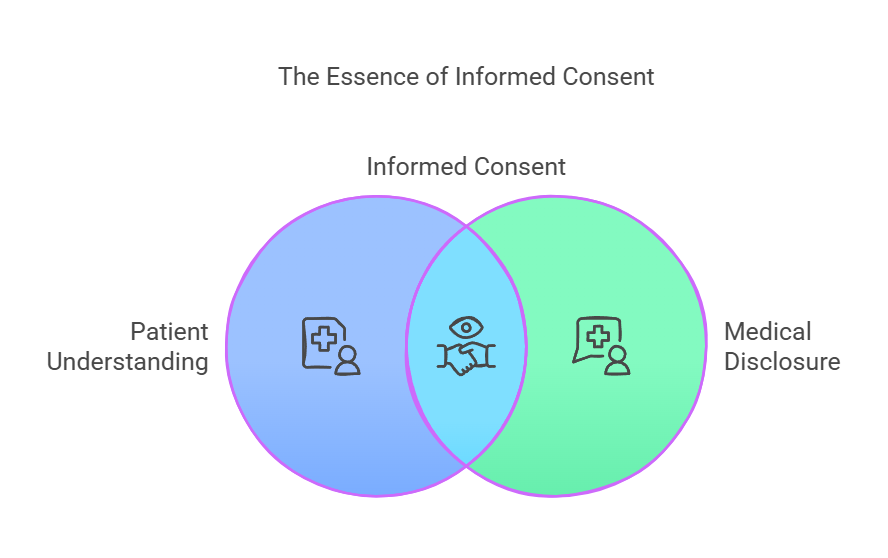
1.2.1 Legal Issues in Informed Consent
-
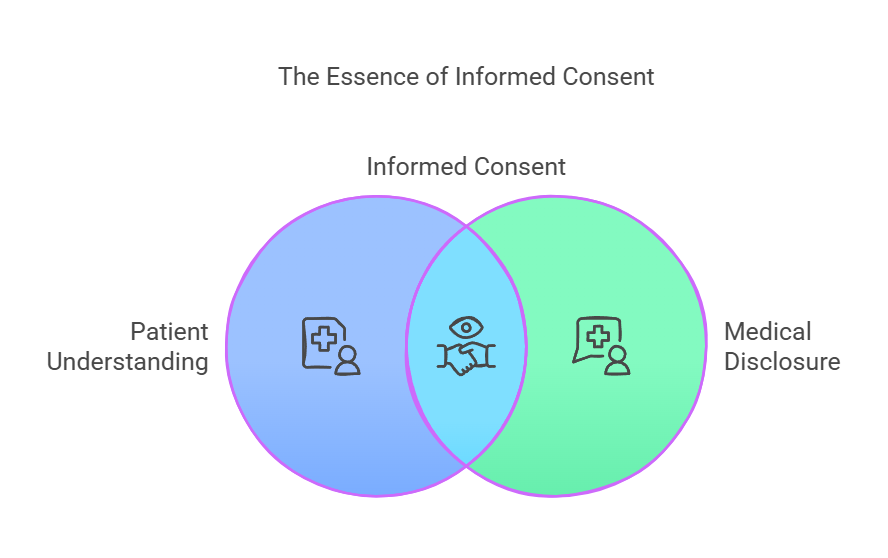
Informed consent is a legal requirement that ensures
patients understand the risks, benefits, and alternatives to a proposed
treatment or intervention.
-
Nurses must ensure that consent is obtained voluntarily and that patients
have the capacity to make decisions.
-
Failure to secure informed consent can lead to legal repercussions for
healthcare providers.
1.2.2 Legal Rights and Responsibilities of Health Educators
-
Health educators have the legal responsibility to provide accurate and
evidence-based information to patients.
-
They must also respect patient confidentiality and privacy as mandated by
laws such as the Health Insurance Portability and Accountability Act
(HIPAA).
-
Understanding these legal frameworks helps prevent malpractice and protects
both the patient and the educator.
Key Definitions
-
Beneficence: The ethical principle of acting in the best
interest of the patient.
-
Non-maleficence: The ethical principle of “do no harm’’.
-
Justice: The ethical principle of fairness and equality in
healthcare.
-
Autonomy: The right of patients to make informed choices
about their care.
-
Informed Consent: The process of obtaining permission from
patients after providing necessary information.

Key Principles
-
Ethical principles guide the practice of nursing, ensuring patient welfare
and rights are prioritized.
-
Legal considerations protect both patients and healthcare providers,
establishing clear expectations and responsibilities.
Relevance to the PNLE Exam
-
Understanding ethical and legal foundations is crucial as these topics
frequently appear in PNLE questions, particularly in scenarios involving
patient rights and decision-making.
Quick Tips
-
Remember the acronym B.J.A. for ethical principles:
Beneficence, Justice,
Autonomy.
-
Always ensure informed consent is documented to protect yourself legally.
Common Misconceptions
-
Some may confuse beneficence with
non-maleficence, thinking they are interchangeable;
however, beneficence focuses on promoting good, while non-maleficence
focuses on avoiding harm.
Practice Questions
-
Which ethical principle requires nurses to act in the best interest of
the patient?
- A) Justice
- B) Non-maleficence
- C) Beneficence
- D) Autonomy
Correct Answer: C) Beneficence
Rationale: Beneficence is specifically about promoting the
well-being of patients.
2. What is required for informed consent to be valid?
- A) The patient must be informed of the treatment only.
- B) The patient must understand the information provided.
- C) The patient must agree to the treatment without questions.
- D) The patient must be a family member.
Correct Answer: B) The patient must understand the information
provided.
Rationale: Understanding is crucial for informed
consent to be valid.
Take-Home Message
Ethical and legal foundations are essential in nursing education, ensuring that
patient rights are respected and upheld while promoting their well-being.
2. Evidence-Based Practices Related to Health Education
2.1 Developing Evidence-Based Programs
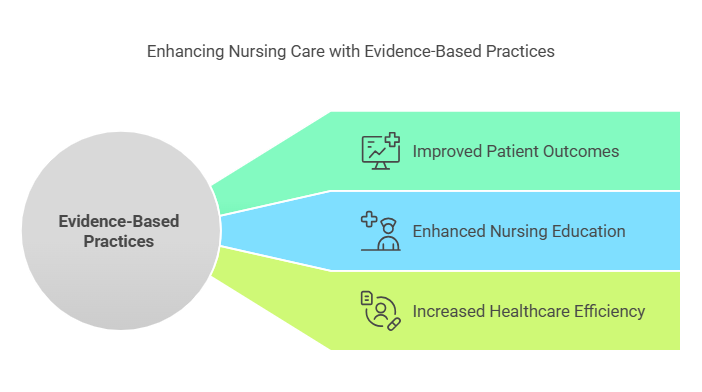
2.1.1 Aligning Education with Evidence
-
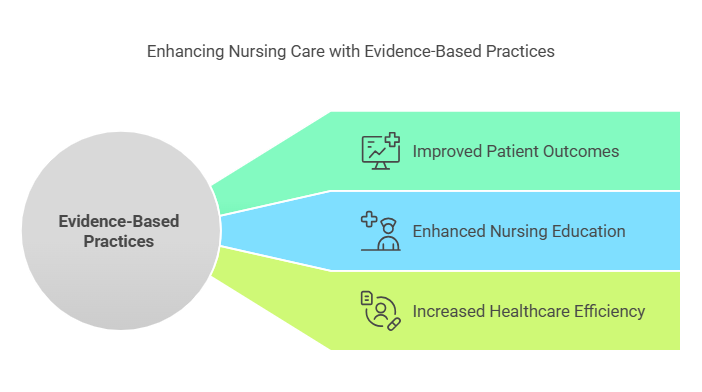
Overview: Aligning education with evidence involves
integrating the best available research with clinical expertise and patient
values. This ensures that health education programs are relevant and
effective.
- Key Definitions:
-
Evidence-Based Practice (EBP): A problem-solving approach
to decision-making that integrates the best available evidence, clinical
expertise, and patient preferences.
-
Clinical Expertise: The skills and past experiences of
healthcare professionals that inform their decisions.
- Key Principles:
- Utilize current research to guide curriculum development.
- Engage stakeholders in the design process to ensure relevance.
- Continuously update educational materials based on new evidence.
2.1.2 Evaluating Educational Interventions
-
Overview: Evaluating educational interventions is crucial
for determining their effectiveness and making necessary adjustments.
- Key Definitions:
-
Outcome Evaluation: Assessment of the changes in
knowledge, attitudes, or behaviors resulting from an educational program.
-
Process Evaluation: Examination of the implementation of
the program to ensure fidelity to the design.
- Key Principles:
- Use both qualitative and quantitative methods to assess outcomes.
- Gather feedback from participants to improve future interventions.
- Establish clear metrics for success prior to implementation.
2.2 Importance of Evidence-Based Practice
2.2.1 Use of Research in Health Education
-
Overview: Research is fundamental in shaping health
education, ensuring that information disseminated is accurate and effective.
- Key Definitions:
-
Research Utilization: The process of incorporating
research findings into practice.
-
Best Practices: Evidence-based methods that have been
proven effective through research.
- Key Principles:
- Stay updated with the latest research findings.
-
Encourage critical thinking among students regarding the application of
research.
2.2.2 Incorporating Current Research Findings
-
Overview: Incorporating current research findings into
health education enhances the credibility and reliability of the information
provided.
- Key Definitions:
-
Translational Research: Research that aims to translate
findings from basic science into practical applications.
-
Systematic Review: A comprehensive summary of existing
research on a particular topic.
- Key Principles:
-
Regularly review and integrate new research into educational content.
-
Foster a culture of inquiry and continuous learning among educators and
students.
Relevance to the PNLE Exam
-
Understanding the principles of EBP is critical as questions related to
evidence-based nursing practices are frequently tested.
-
Focus on the application of research in clinical settings, as this is a
common area of examination.
Practice Questions
-
Which of the following best defines Evidence-Based Practice
(EBP)?
- A) A method based solely on clinical experience.
-
B) A decision-making process that incorporates research evidence, clinical
expertise, and patient preferences.
- C) A practice that relies on traditional methods.
- D) A system of care that does not require research.
Correct Answer: B) A decision-making process that incorporates
research evidence, clinical expertise, and patient preferences.
Rationale: EBP combines multiple sources of information to
ensure effective care.
-
What is the primary purpose of evaluating educational
interventions?
- A) To determine the cost-effectiveness of the program.
-
B) To assess the implementation process and outcomes for improvement.
- C) To compare different educational models.
- D) To collect data for future research.
Correct Answer: B) To assess the implementation process and
outcomes for improvement.
Rationale: Evaluation focuses on
understanding the effectiveness and fidelity of educational programs.
Quick Tips
-
Remember the acronym PICO (Population, Intervention,
Comparison, Outcome) to formulate clinical questions related to EBP.
-
Keep abreast of the latest research by subscribing to nursing journals and
attending relevant workshops.
Take-Home Message
Integrating evidence-based practices into health education is essential for
enhancing the quality and effectiveness of nursing care.
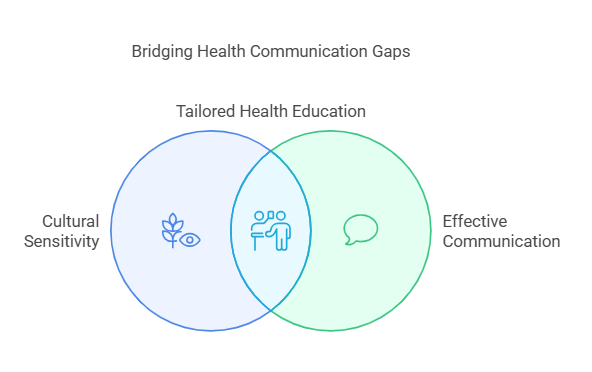
3. Filipino Cultural Characteristics and Health Care Beliefs
3.1 Cultural Sensitivity in Health Education
Cultural sensitivity is crucial in nursing practice, especially when addressing
the diverse beliefs and practices of Filipino patients. Understanding cultural
nuances can significantly enhance patient education and compliance.
3.1.1 Addressing Language Barriers
- Key Definitions:
-
Language Barrier: A communication obstacle that occurs
when individuals do not share a common language.
-
Cultural Competence: The ability to understand,
communicate with, and effectively interact with people across cultures.
- Key Principles:
- Utilize interpreters or bilingual staff when necessary.
- Employ visual aids and simple language to enhance understanding.
- Encourage patients to express their concerns and preferences.
-
Relevance to the PNLE Exam: Language barriers are
frequently tested in scenarios involving patient education and communication
strategies.
-
Practice Question: Which of the following is the best
approach to overcome language barriers in patient education?
- A) Speak louder to the patient
- B) Use medical jargon
- C) Utilize a professional interpreter
- D) Assume the patient understands
Correct Answer: C) Utilize a professional interpreter.
Rationale: This ensures accurate communication and
understanding of health information.
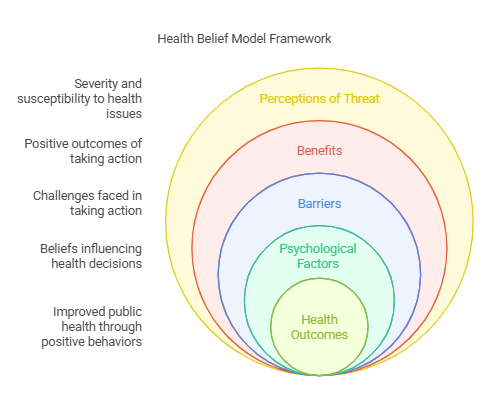
3.1.2 Health Belief Models
- Key Definitions:
-
Health Belief Model: A psychological model that attempts
to explain and predict health behaviors by focusing on attitudes and
beliefs of individuals.
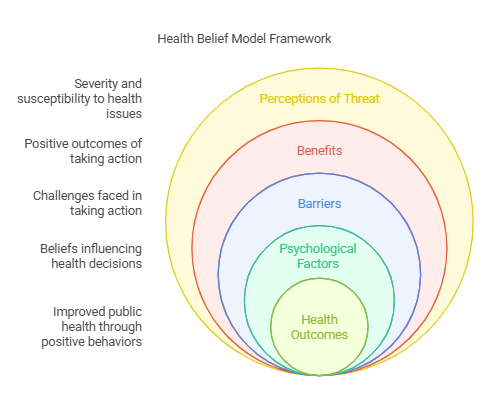
- Key Principles:
- Assess patients’ perceptions of susceptibility to health issues.
- Address perceived benefits and barriers to health actions.
- Enhance self-efficacy to encourage health-promoting behaviors.
-
Common Misconceptions: Many believe that providing
information alone will change health behaviors; however, understanding
beliefs and attitudes is essential.
3.2 Common Filipino Health Beliefs
Filipino health beliefs often blend traditional and modern practices,
influencing health-seeking behavior.
3.2.1 Folk Medicine and Traditional Healing
- Key Definitions:
-
Folk Medicine: Traditional healing practices based on
cultural beliefs and practices.
-
Herbal Remedies: Use of plants for medicinal purposes,
common in Filipino culture.

- Key Principles:
-
Recognize the role of traditional healers (e.g.,
albularyo) in the community.
-
Understand the importance of herbal medicine in patient preferences.
-
Quick Tips: Always inquire about any traditional remedies
patients may be using to avoid potential interactions with prescribed
medications.
3.2.2 Family as a Health Unit
- Key Definitions:
-
Family-Centered Care: An approach that recognizes the
family as the primary unit of care.

- Key Principles:
- Involve family members in health education and decision-making.
- Acknowledge the family’s role in supporting the patient’s health.
-
Connection: This contrasts with more individualistic
approaches common in Western healthcare systems, emphasizing the collective
over the individual.
Take-Home Message
Understanding Filipino cultural characteristics and health care beliefs is
essential for providing effective, culturally sensitive nursing care that
promotes better health outcomes.
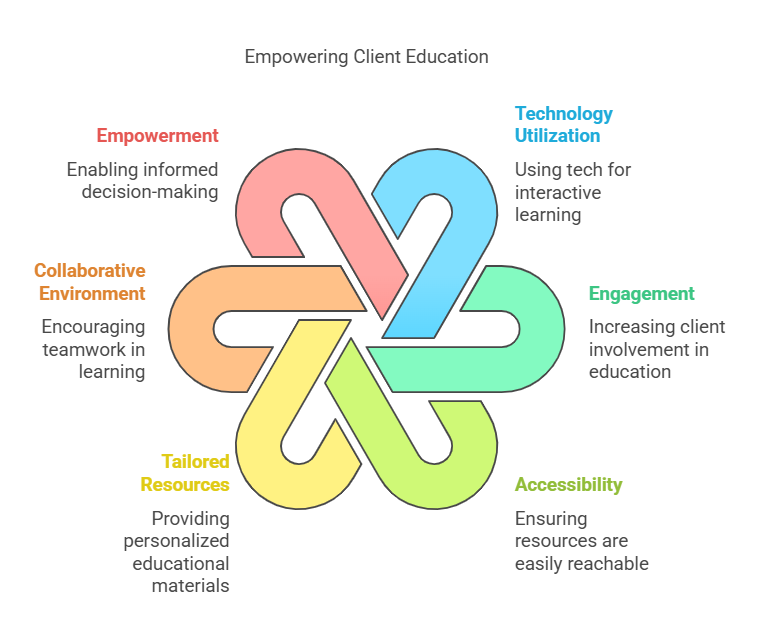
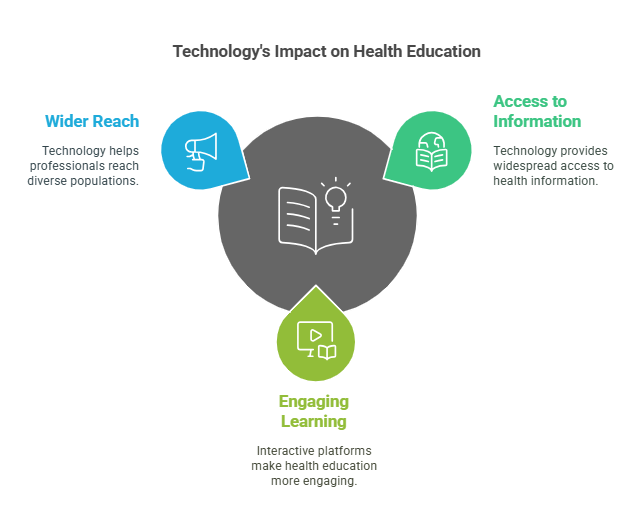
4. Future Directions for Client Education
4.1 Emerging Trends in Health Education
The landscape of health education is rapidly evolving, driven by advancements in
technology and innovative teaching methodologies. Understanding these trends is
crucial for nursing professionals to effectively educate clients and promote
better health outcomes.
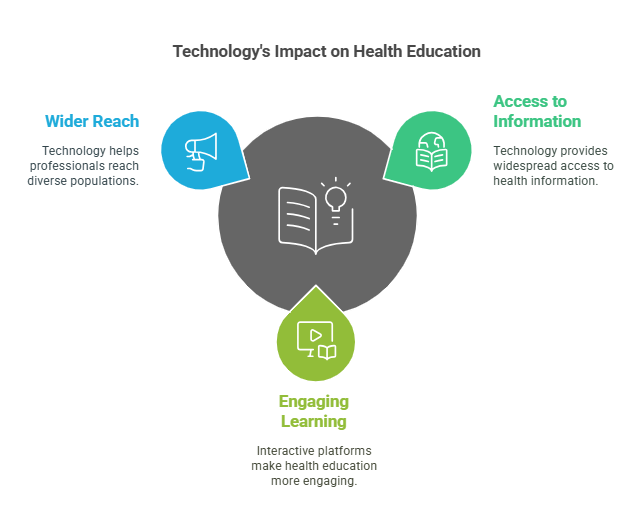
4.1.1 Technology in Health Education
-
Telehealth: The use of telecommunications technology to
provide healthcare services remotely, enhancing access to care.
-
Mobile Health (mHealth): The integration of mobile devices
in health education, allowing for real-time communication and information
dissemination.
-
E-learning Platforms: Online resources that facilitate
self-paced learning for clients, making health education more accessible.
Key Definitions:
-
Telehealth: Remote healthcare services provided through
digital communication tools.
-
mHealth: Health services delivered via mobile devices.
-
E-learning: Learning conducted via electronic media,
typically on the Internet.
Key Principles:
-
Accessibility: Ensuring that health education resources are
available to all clients, regardless of location.
-
Engagement: Utilizing interactive technologies to enhance
client participation in their health education.
-
Personalization: Tailoring health education materials to
meet the individual needs of clients.
4.1.2 New Teaching Technologies
-
Virtual Reality (VR): Immersive simulations that allow
clients to experience health scenarios in a controlled environment.
-
Augmented Reality (AR): Overlaying digital information onto
the real world to enhance learning experiences.
-
Gamification: Incorporating game-like elements in education
to motivate clients and improve learning outcomes.
Relevance to the PNLE Exam:
-
Familiarity with these emerging technologies is increasingly tested in the
PNLE, especially regarding their application in client education and health
promotion.
Common Misconceptions:
-
Misconception: Technology replaces the need for personal
interaction in health education.
-
Clarification: Technology enhances but does not replace
the importance of personal connections in client education.
Practice Questions:
-
Which of the following best describes telehealth?
- A) In-person consultations only
- B) Remote healthcare services via digital tools
- C) Traditional classroom education
- D) Group therapy sessions
Correct Answer: B) Remote healthcare services via digital tools
Rationale: Telehealth specifically refers to the delivery of
healthcare services through telecommunications technology.
-
What is a key benefit of using gamification in health education?
- A) It reduces the need for client participation.
- B) It discourages learning.
- C) It increases motivation and engagement.
- D) It complicates the learning process.
Correct Answer: C) It increases motivation and engagement.
Rationale: Gamification leverages game-like elements to make
learning more enjoyable and engaging for clients.
Quick Tips:
-
Stay updated on technological advancements in health education to enhance
your teaching strategies.
-
Utilize interactive tools to foster client engagement and improve knowledge
retention.
Take-Home Message:
Embracing emerging technologies in health education is essential for nursing
professionals to enhance client engagement and promote effective learning
outcomes.”
5. Health Education Process
5.1 Planning Health Education
The planning phase is crucial in developing effective health education programs
that cater to the needs of the target population. This involves setting clear
objectives and designing a comprehensive health education plan.
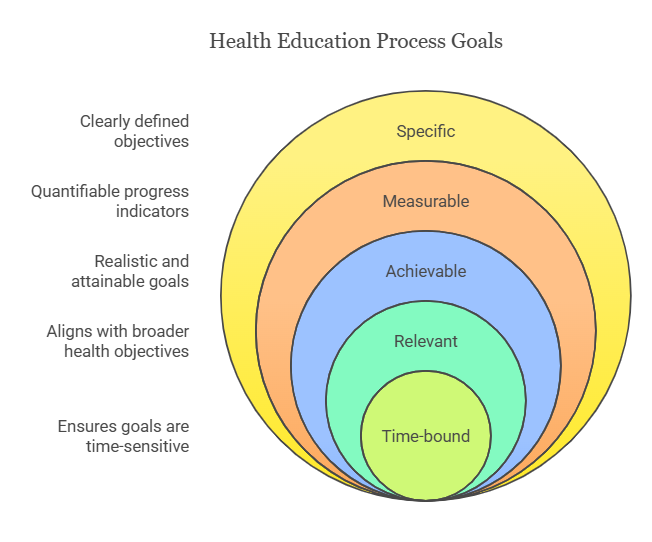
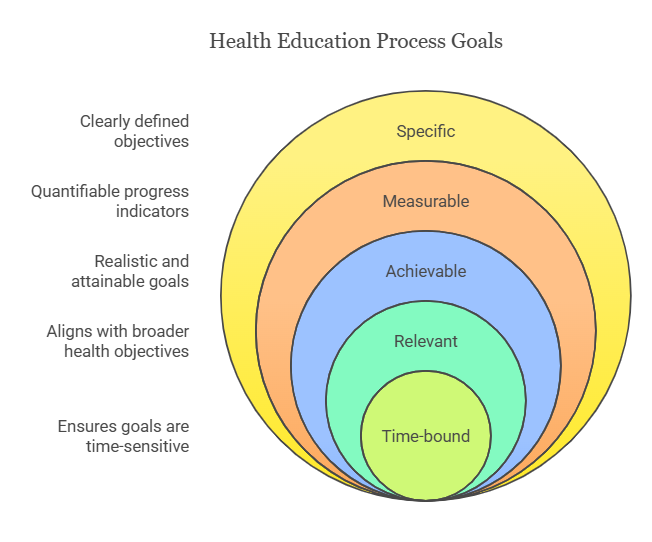
5.1.1 Setting Objectives
-
Objectives should be
Specific, Measurable, Achievable, Relevant, and Time-bound
(SMART).
-
Clearly defined objectives guide the direction of the health education
initiative and help in evaluating its success.
Key Definitions:
-
SMART Objectives: A framework for setting clear and
attainable goals in health education.
Key Principles:
-
Involve stakeholders in the objective-setting process to ensure relevance
and buy-in.
- Align objectives with the health needs of the community.
Relevance to the PNLE Exam:
-
Expect questions on the formulation of SMART objectives and their importance
in health education.
5.1.2 Designing a Health Education Plan
-
A well-structured health education plan outlines the content, methods, and
resources needed for effective delivery.
-
Consider the learning styles of the target audience to
enhance engagement and retention.
Key Definitions:
-
Health Education Plan: A strategic document that details
how health education will be delivered.
Key Principles:
-
Utilize a variety of teaching methods (e.g., lectures, workshops,
demonstrations) to cater to diverse learning preferences.
- Incorporate feedback mechanisms to continuously improve the plan.
Quick Tips:
-
Always assess the needs of your audience before designing your plan to
ensure it is relevant and effective.
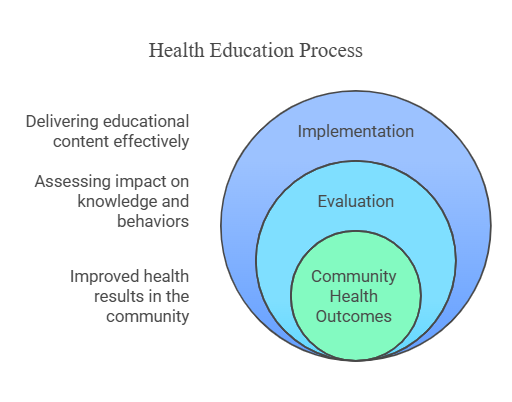
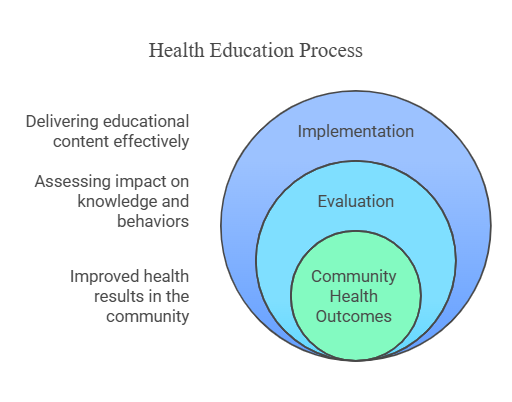
5.2 Implementation and Evaluation
The implementation phase involves delivering the health education sessions,
while evaluation assesses the effectiveness of the program.
5.2.1 Delivering Effective Sessions
-
Engage participants through interactive activities and discussions to
promote active learning.
-
Ensure that the environment is conducive to learning, free from
distractions.
Key Definitions:
-
Effective Session Delivery: The process of presenting
health education content in a way that maximizes participant engagement and
understanding.
Key Principles:
-
Use clear and concise language, avoiding jargon that may confuse the
audience.
-
Adapt your teaching style based on real-time feedback during sessions.
Practice Question:
- Which of the following is NOT a characteristic of SMART objectives?
- A) Specific
- B) Measurable
- C) Ambiguous
- D) Time-bound
Correct Answer: C) Ambiguous
Rationale:
SMART objectives must be specific and clear to guide effective health education.
5.2.2 Measuring Educational Outcomes
-
Evaluation should focus on both process (how the education was delivered)
and outcomes (what participants learned).
-
Use tools such as surveys, quizzes, and interviews to assess the
effectiveness of the health education program.
Key Definitions:
-
Educational Outcomes: The knowledge, skills, and attitudes
gained by participants as a result of the health education program.
Key Principles:
-
Establish baseline data before the program to measure changes effectively.
-
Continuous evaluation allows for real-time adjustments to improve future
sessions.
Common Misconceptions:
-
Many believe that evaluation is only necessary at the end of a program;
however, ongoing assessment is crucial for continuous improvement.
Take-Home Message: Effective health education requires careful
planning, engaging delivery, and thorough evaluation to ensure that objectives
are met and participants benefit.
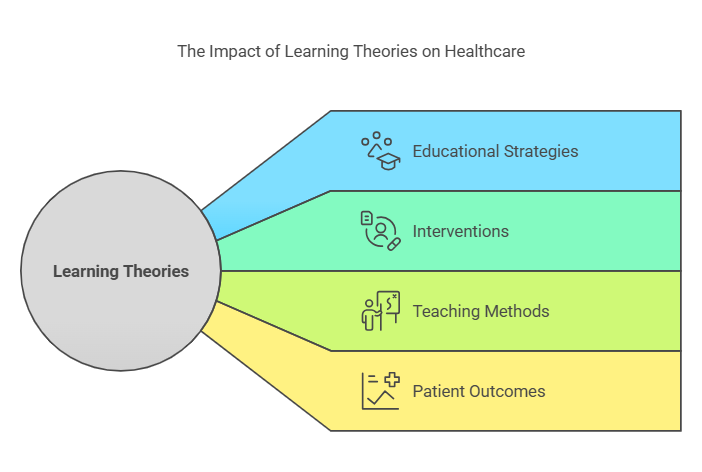
6. Learning Theories Related to Health Care Practice
This section explores essential learning theories that inform health care
education and practice. Understanding these theories is vital for nursing
professionals to effectively educate patients and enhance their own learning.
6.1 Adult Learning Principles
-
Overview: Adult learning principles, often referred to as
andragogy, emphasize the unique needs of adult learners. Unlike children,
adults bring prior experiences and self-directed learning capabilities to
the educational process.
- Key Definitions:
-
Andragogy: The method and practice of teaching adult
learners.
-
Self-Directed Learning: A process in which individuals
take the initiative in diagnosing their learning needs, formulating goals,
identifying resources, and evaluating learning outcomes.
- Key Principles:
- Adults need to know why they are learning something.
-
Adults bring life experiences and knowledge to the learning process.
-
Adults are goal-oriented and expect to be involved in the planning and
evaluation of their instruction.
-
Adults are relevancy-oriented and need to see the immediate applicability
of what they are learning.
- Relevance to the PNLE Exam:
-
Understanding adult learning principles is crucial for nursing education,
particularly in patient education scenarios. Expect questions on how to
tailor teaching strategies to adult learners.
- Practice Question:
- Which of the following is a principle of adult learning?
- A) Adults learn best through rote memorization.
- B) Adults need to know the reason for learning.
- C) Adults prefer passive learning environments.
- D) Adults do not bring prior experiences to learning.
Correct Answer: B) Adults need to know the reason for learning.
Rationale: This principle emphasizes the importance of
relevance in adult education.
6.2 Social Learning Theory
-
Overview: Proposed by Albert Bandura, Social Learning
Theory posits that learning occurs through observation, imitation, and
modeling. It highlights the importance of social interaction and the
environment in the learning process.
- Key Definitions:
-
Observational Learning: Learning that occurs through
observing the behaviors of others.
-
Modeling: The process of learning behaviors by watching
others.
- Key Principles:
- Learning is a social process.
- Individuals can learn new behaviors by observing others.
-
Reinforcement and punishment influence the likelihood of behavior being
repeated.
- Common Misconceptions:
-
Some may confuse Social Learning Theory with behaviorism, but the former
emphasizes cognitive processes and social context, while the latter
focuses solely on observable behaviors.
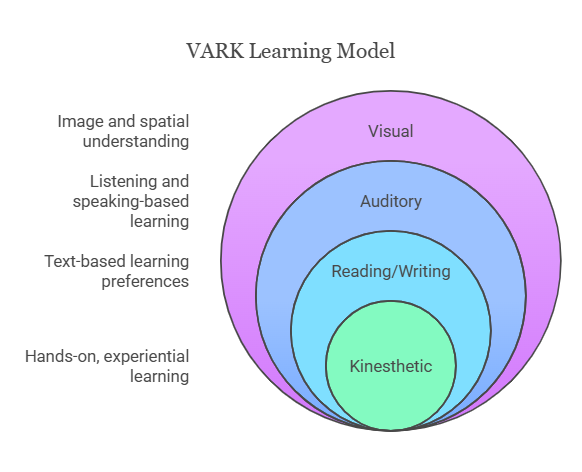
6.3 VARK Model
-
Overview: The VARK Model categorizes learners based on
their preferred sensory modalities: Visual, Auditory, Reading/Writing, and
Kinesthetic. This model helps educators tailor their teaching strategies to
meet diverse learning preferences.
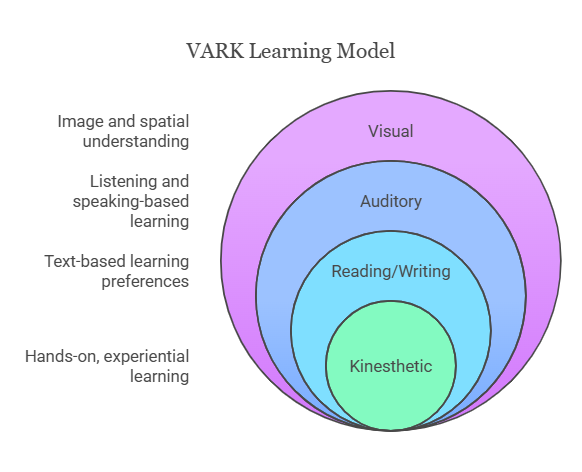
- Key Definitions:
-
Visual Learners: Prefer to see and visualize information.
- Auditory Learners: Learn best through listening.
-
Reading/Writing Learners: Prefer to engage with text.
-
Kinesthetic Learners: Learn through hands-on experiences.
- Key Principles:
- Different learners require different teaching methods.
- Incorporating multiple modalities can enhance learning outcomes.
- Quick Tips:
-
To remember the VARK categories, think of the acronym VARK itself,
associating each letter with its corresponding learning style.
- Practice Question:
-
A nurse educator is planning a lesson for a group of students with varying
learning preferences. Which of the following strategies would best
accommodate all learning styles?
- A) Lecture only
- B) Use of videos, discussions, and hands-on activities
- C) Reading assignments only
- D) Group projects only
Correct Answer: B) Use of videos, discussions, and hands-on
activities.
Rationale: This approach incorporates visual,
auditory, and kinesthetic learning styles.
Take-Home Message
Understanding and applying learning theories enhances nursing education and
patient care, ensuring that both nurses and patients can effectively engage in
the learning process.
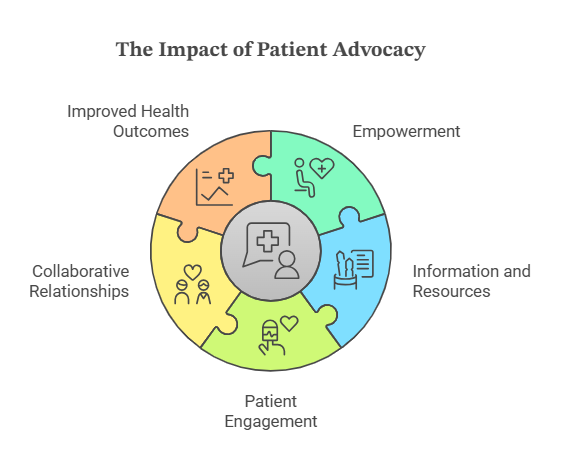
7. Patient Advocacy in Health Education
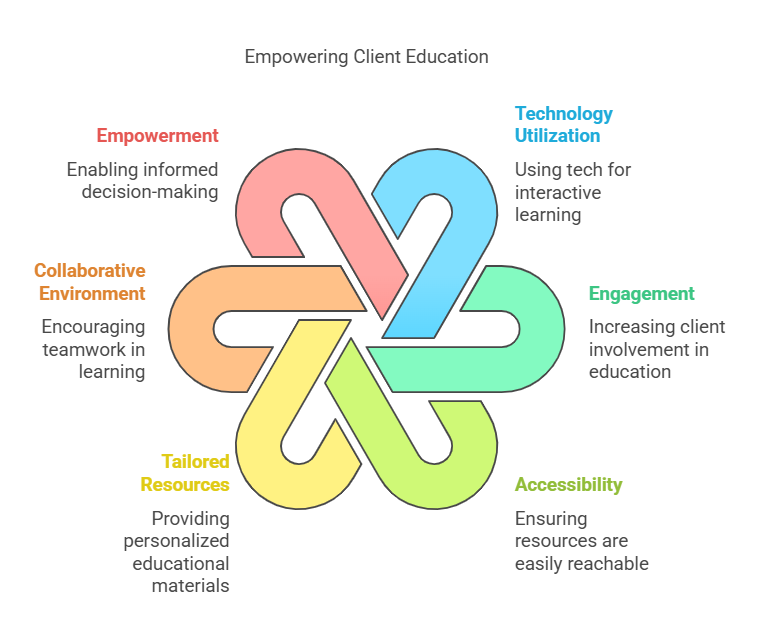
7.1 Empowering Patients
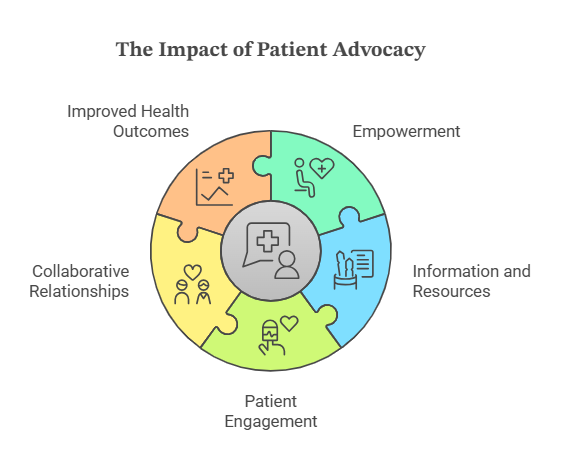
-
Patient empowerment is the process of enabling patients to
take control of their health and make informed decisions regarding their
care.
-
Key strategies include providing clear information,
encouraging self-management, and fostering
shared decision-making between patients and healthcare
providers.
 Key Definitions:
Key Definitions:
-
Patient Empowerment: The process by which patients gain the
knowledge, skills, and confidence to manage their own health.
-
Shared Decision-Making: A collaborative process that allows
patients and their healthcare providers to make health decisions together.
Key Principles:
-
Informed Consent: Patients must be adequately informed
about their treatment options to make choices that align with their values
and preferences.
-
Respect for Autonomy: Acknowledging and respecting
patients’ rights to make their own healthcare decisions.
Relevance to the PNLE Exam:
-
Understanding patient empowerment is crucial as it aligns with the
principles of patient-centered care, a frequent topic in PNLE.
Practice Question:
- What is the primary goal of patient empowerment in healthcare?
- A) To increase healthcare costs
- B) To enhance patient compliance
- C) To enable patients to make informed decisions
- D) To reduce the workload of healthcare providers
Correct Answer: C) To enable patients to make informed
decisions
Rationale: Patient empowerment focuses on
providing patients with the necessary tools and information to take charge of
their health.
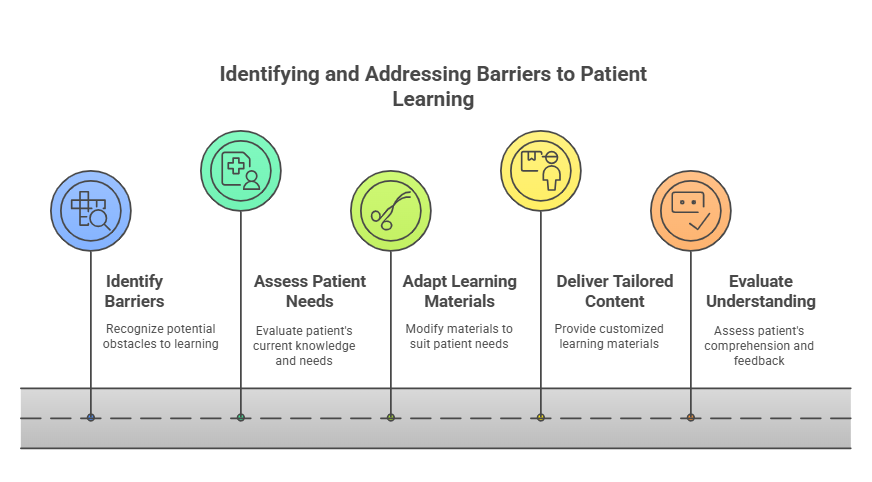
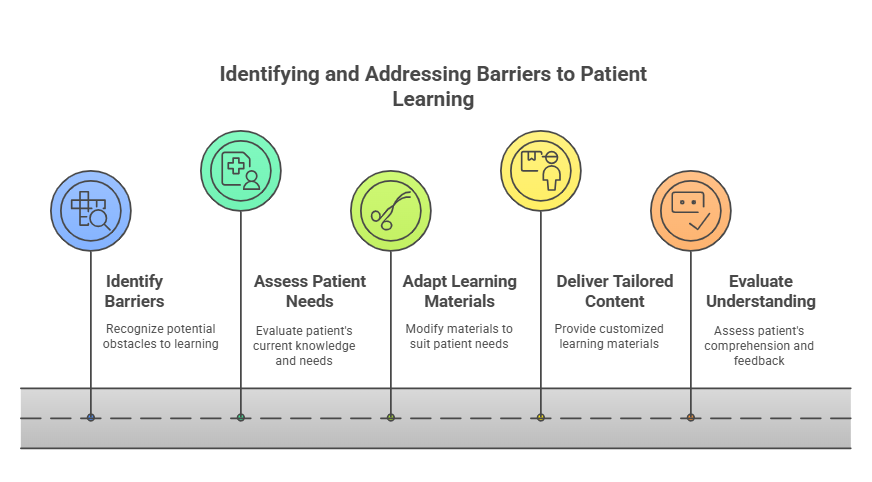
7.2 Overcoming Barriers to Learning
-
Barriers to learning can include cognitive limitations,
language differences, cultural beliefs,
and lack of resources.
-
Strategies to overcome these barriers involve using
plain language, employing visual aids, and
adapting educational materials to meet diverse needs.
Key Definitions:
-
Barriers to Learning: Factors that impede a patient’s
ability to understand or retain health information.
-
Cultural Competence: The ability of healthcare providers to
understand and respect cultural differences in patient populations.
Key Principles:
-
Tailored Education: Customize health education to fit the
unique needs of each patient.
-
Active Engagement: Encourage active participation from
patients in their learning process.
Common Misconceptions:
-
It is often assumed that all patients understand medical terminology;
however, many patients may require simplified explanations.
Quick Tips:
-
Always assess a patient’s understanding by asking them to explain back what
they have learned.
- Utilize teach-back methods to confirm comprehension.
Take-Home Message
Empowering patients through effective education and overcoming learning barriers
is essential for fostering autonomy and improving health outcomes.
8. Teaching Strategies in Health Education
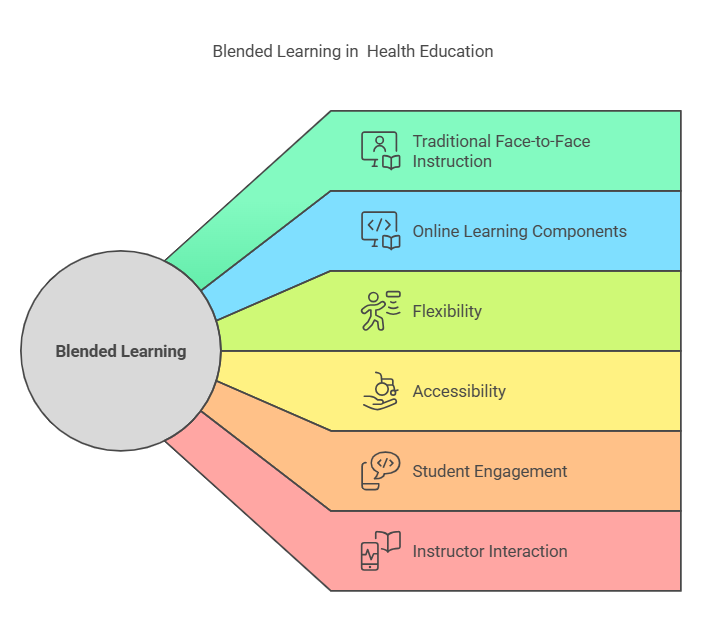
8.1 Blended Learning
-
Overview: Blended learning combines traditional
face-to-face instruction with online learning activities. This approach
allows for flexibility in teaching and learning, catering to diverse student
needs.
- Key Definitions:
-
Blended Learning: An educational approach that integrates
online digital media with traditional classroom methods.
-
Asynchronous Learning: Learning that does not occur in
the same place or at the same time, allowing students to engage with
materials at their own pace.
- Key Principles:
-
Flexibility: Students can choose when and where to engage
with course materials.
-
Personalization: Tailoring learning experiences to meet
individual student needs.
-
Engagement: Utilizing various multimedia tools to enhance
student interaction and motivation.
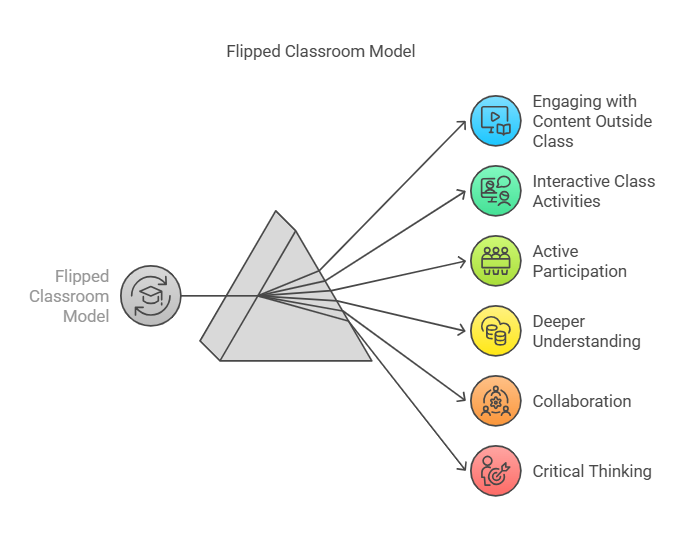
8.2 Flipped Classroom
-
Overview: The flipped classroom model reverses traditional
teaching methods by delivering instructional content online outside of the
classroom and moving activities into the classroom.
 Key Definitions :
Key Definitions :
-
Flipped Classroom: An instructional strategy where students
learn content at home and apply knowledge in class through interactive
activities.
-
Active Learning: An approach that actively engages students
in the learning process, encouraging them to participate in discussions and
problem-solving.
Key Principles:
-
Preparation: Students prepare by reviewing materials before
class.
-
Application: Class time is used for discussions,
problem-solving, and collaborative projects.
-
Feedback: Immediate feedback is provided during class
activities, enhancing understanding.
8.3 Group Discussions and Role-Playing
-
Overview: Group discussions and role-playing are
interactive strategies that promote critical thinking and communication
skills among students.
- Key Definitions:
-
Group Discussion: A collaborative dialogue among students
to explore a particular topic or issue.
-
Role-Playing: A technique where students act out
scenarios to practice skills and understand different perspectives.
- Key Principles:
- Collaboration: Encourages
- teamwork and sharing of ideas.
-
Perspective-Taking: Helps students understand various
viewpoints and develop empathy.
-
Skill Development: Enhances communication, negotiation,
and problem-solving skills.
Relevance to the PNLE Exam
-
Understanding these teaching strategies is crucial for the PNLE, as they are
often integrated into nursing education. Questions may focus on identifying
the benefits of each strategy or scenarios where they would be most
effective.
Common Misconceptions
-
Blended Learning vs. Flipped Classroom: Many confuse these
two concepts. While blended learning includes both online and in-person
components, the flipped classroom specifically involves students learning
content at home and engaging in activities during class.
Practice Questions
-
Which of the following best describes blended learning?
- A) Learning that occurs only in the classroom.
- B) A combination of online and traditional learning.
- C) Learning that happens in groups only.
- D) None of the above.
Correct Answer: B) A combination of online and traditional
learning.
Rationale: Blended learning integrates both
online and face-to-face instruction, enhancing flexibility and engagement.
-
In a flipped classroom, students are expected to:
- A) Learn new content during class time.
- B) Review instructional materials at home before class.
- C) Participate in group discussions only.
- D) None of the above.
Correct Answer: B) Review instructional materials at home
before class.
Rationale: The flipped classroom model
emphasizes learning content at home, allowing class time for application and
interaction.
Quick Tips
-
Remember the acronym BFG for the three strategies:
Blended Learning, Flipped Classroom,
Group Discussions/Role-Playing.
-
Keep in mind that engagement and interaction are key components of effective
health education strategies.
Take-Home Message
Effective teaching strategies such as blended learning, flipped classrooms, and
interactive discussions are essential for fostering a dynamic learning
environment in health education.
9. Interdisciplinary Collaboration in Health Education
9.1 Multidisciplinary Teamwork
-
Multidisciplinary teamwork involves various professionals
from different disciplines working together towards a common goal in health
education.
-
This approach enhances patient care by integrating diverse expertise,
ensuring comprehensive health education and improved health outcomes.
Key Definitions:
-
Interdisciplinary Collaboration: A process where
professionals from different fields work together, sharing knowledge and
skills to achieve a common goal.
-
Multidisciplinary Team: A group of professionals from
various specialties who collaborate but maintain their distinct roles.
Key Principles:
-
Communication: Effective communication is vital for sharing
information and ensuring all team members are aligned.
-
Respect for Expertise: Each member’s unique skills and
knowledge are valued, fostering a collaborative environment.
-
Shared Goals: Team members work towards common objectives,
enhancing the overall effectiveness of health education.
Relevance to the PNLE Exam:
-
Understanding the dynamics of multidisciplinary teamwork is crucial, as
questions may focus on the roles of various healthcare professionals and the
importance of collaboration in patient education.
Common Misconceptions:
-
Misconception: Multidisciplinary teams work independently
without integrating their knowledge.
-
Clarification: While team members maintain their
specialties, effective collaboration requires integration of their
insights to enhance patient care.
Quick Tips:
-
Remember the acronym C.R.E.S.T. for effective
multidisciplinary teamwork:
- Communication
- Respect
- Expertise
- Shared Goals
- Teamwork
9.2 Role of Nurses in Collaborative Education
-
Nurses play a pivotal role in interdisciplinary collaboration, acting as
liaisons between patients and other healthcare professionals.
-
They facilitate health education by assessing patient needs, delivering
information, and coordinating care plans.
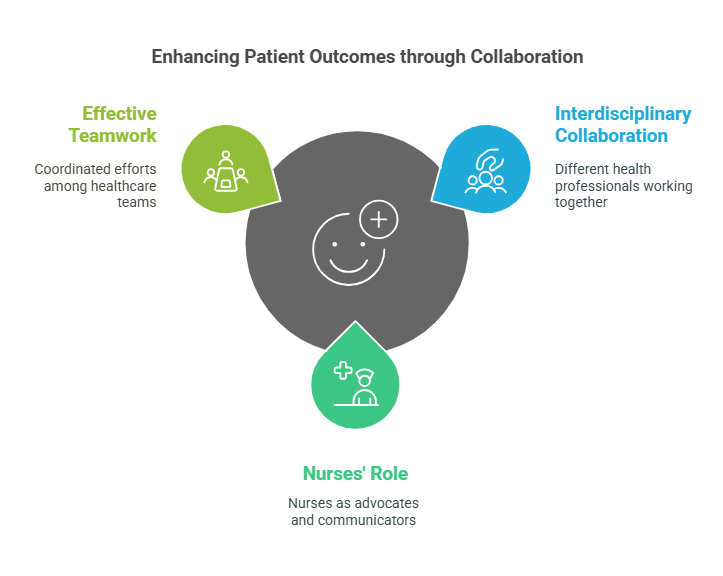
Key Definitions:
-
Patient Advocacy: The role of nurses in representing and
supporting the interests of patients within the healthcare team.
Key Principles:
-
Holistic Care: Nurses consider the physical, emotional, and
social aspects of patient health, ensuring comprehensive education.
-
Continuous Learning: Nurses engage in lifelong learning to
stay updated with best practices in health education and interdisciplinary
collaboration.
Practice Questions:
-
What is the primary goal of interdisciplinary collaboration in health
education?
- A) To maintain individual professional roles
- B) To enhance patient care through shared knowledge
- C) To reduce healthcare costs
- D) To increase competition among professionals
Correct Answer: B) To enhance patient care through shared
knowledge.
Rationale: The primary aim of
interdisciplinary collaboration is to improve patient outcomes by integrating
diverse expertise.
-
Which of the following best describes the role of nurses in collaborative
education?
- A) They only provide direct patient care.
- B) They act as liaisons and advocates for patients.
- C) They focus solely on administrative tasks.
- D) They do not participate in team meetings
Correct Answer: B) They act as liaisons and advocates for
patients.
Rationale: Nurses are integral to facilitating
communication and ensuring that patient needs are met within the healthcare
team.
Take-Home Message
Interdisciplinary collaboration in health education enhances patient outcomes
through effective teamwork, where nurses play a crucial role as advocates and
communicators.
10. Legal and Ethical Considerations in Health Education
This chapter focuses on the critical legal and ethical frameworks that guide
nursing practice, particularly in health education. Understanding these
principles is essential for nursing professionals to ensure patient safety,
uphold professional standards, and navigate complex healthcare environments.
10.1 Confidentiality and Duty of Care
-
Confidentiality refers to the ethical principle that
obligates healthcare professionals to protect patient information from
unauthorized disclosure.
-
Duty of Care is the legal obligation of healthcare
providers to adhere to a standard of reasonable care while performing any
acts that could foreseeably harm patients.
Key Definitions:
-
HIPAA: Health Insurance Portability and Accountability Act,
a U.S. law that mandates the protection of patient health information.
-
Breach of Confidentiality: Unauthorized sharing of patient
information, which can lead to legal consequences.
Key Principles:
- Respect for patient privacy is paramount.
-
Nurses must ensure that patient information is shared only with authorized
individuals.
-
Duty of care requires nurses to act in the best interest of their patients,
providing safe and competent care.
Relevance to the PNLE Exam:
-
Expect questions on scenarios involving breaches of confidentiality and the
implications of duty of care.
- Familiarize yourself with legal cases that highlight these concepts.
Common Misconceptions:
-
Misconception: All patient information can be shared with
family members.
-
Clarification: Information can only be shared with family
members if the patient has given explicit consent.
Quick Tips:
- Always ask for consent before sharing patient information.
-
Remember the acronym C.A.R.E.:
Confidentiality, Accountability,
Respect, Ethics.
10.2 Informed Consent and Professional Boundaries
-
Informed Consent is the process by which a patient
voluntarily agrees to a proposed medical intervention after being fully
informed of the risks, benefits, and alternatives.
-
Professional Boundaries refer to the limits that protect
the space between the nurse’s professional power and the patient’s
vulnerability.
Key Definitions:
-
Autonomy: The right of patients to make their own decisions
regarding their healthcare.
-
Boundary Violation: Any behavior that harms the
nurse-patient relationship, such as personal involvement or inappropriate
communication.
Key Principles:
-
Patients must be provided with all necessary information to make informed
decisions.
-
Nurses must maintain professional boundaries to foster trust and respect in
the nurse-patient relationship.
Relevance to the PNLE Exam:
-
Questions may focus on scenarios requiring informed consent and identifying
boundary violations.
- Understanding the legal implications of informed consent is crucial.
Practice Questions:
-
A nurse discusses a patient’s treatment plan with the patient’s family
without the patient’s consent. This is an example of:
- A) Ethical practice
- B) Breach of confidentiality
- C) Informed consent
- D) Duty of care
Correct Answer: B – Breach of confidentiality occurs when
patient information is shared without consent.
-
Which of the following is essential for obtaining informed
consent?
- A) The patient is coerced into making a decision.
- B) The patient is provided with all relevant information.
- C) The nurse decides what is best for the patient.
- D) The patient is not informed of the risks involved.
Correct Answer: B – Informed consent requires that the patient
is fully informed before agreeing to treatment.
Take-Home Message
Understanding and applying legal and ethical principles in nursing practice is
essential for ensuring patient safety and maintaining professional integrity.
11. Technology Integration in Health Education
11.1 E-learning and Mobile Health Apps
-
E-learning refers to the use of electronic technologies to
access educational curriculum outside of a traditional classroom. It
provides flexibility and accessibility for nursing students to learn at
their own pace.
-
Mobile health apps are applications designed for
smartphones and tablets that assist in health education, patient management,
and self-care. They can provide information, track health metrics, and
facilitate communication between patients and healthcare providers.
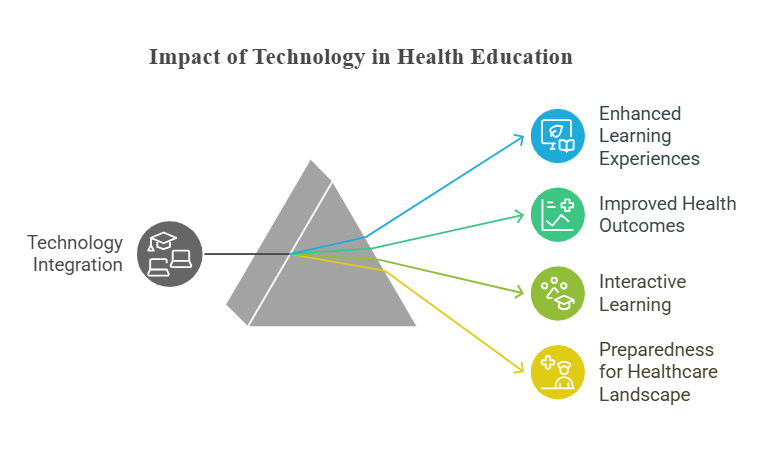
Key Definitions:
-
E-learning: Educational content delivered via electronic
media, often through the internet.
-
Mobile Health Apps: Software applications that support
health management and education through mobile devices.
Key Principles:
-
Accessibility: E-learning and mobile apps make education
more accessible to diverse populations.
-
Interactivity: These technologies promote active learning
through interactive modules and real-time feedback.
-
Personalization: Mobile apps can tailor health education
based on individual user needs and preferences.
Relevance to the PNLE Exam:
-
Understanding the role of technology in health education is crucial as it
reflects current trends in nursing practice and patient education methods.
Expect questions on the advantages and limitations of e-learning and mobile
health applications.
Practice Questions:
-
Which of the following is a primary benefit of e-learning in nursing
education?
- A) Limited access to resources
- B) Flexibility in learning pace
- C) Increased classroom attendance
- D) Standardized testing only
Correct Answer: B – E-learning allows students to learn at
their own pace, accommodating different learning styles.
-
Mobile health apps primarily enhance patient education by:
- A) Providing a platform for social media
- B) Offering personalized health tracking
- C) Replacing healthcare providers
- D) Limiting patient access to information
Correct Answer: B – Mobile health apps offer personalized
health tracking, which empowers patients in managing their health.
11.2 Virtual Reality and Telemedicine
-
Virtual Reality (VR) in health education provides immersive
experiences that can simulate clinical scenarios, enhancing skills and
decision-making in a safe environment.
-
Telemedicine allows healthcare providers to consult with
patients remotely, improving access to care and facilitating ongoing patient
education.
Key Definitions:
-
Virtual Reality (VR): A simulated experience that can be
similar to or completely different from the real world, often used for
training and education.
-
Telemedicine: The remote diagnosis and treatment of
patients through telecommunications technology.
Key Principles:
-
Simulation: VR offers realistic simulations that enhance
learning and retention of clinical skills.
-
Remote Access: Telemedicine breaks geographical barriers,
allowing patients to receive care and education from anywhere.
Common Misconceptions:
-
Many believe that telemedicine replaces in-person visits entirely; however,
it is meant to complement traditional healthcare, providing additional
options for patient care.
Quick Tips:
-
Remember the acronym E-M-V-T for key technologies in health
education: E-learning, Mobile apps, Virtual reality, Telemedicine.
-
Stay updated on the latest apps and technologies to enhance your nursing
practice and patient education strategies.
Take-Home Message:
Technology integration in health education enhances accessibility,
interactivity, and personalization, ultimately improving patient outcomes and
nursing practice.
12. Public Health Interventions
12.1 Epidemic Management (COVID-19)
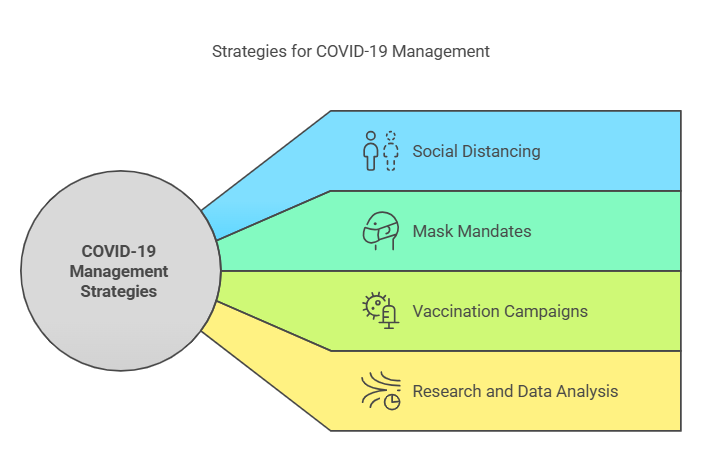
-
Overview: This section discusses the strategies and
measures implemented to manage the COVID-19 pandemic, highlighting the role
of nurses in public health interventions.
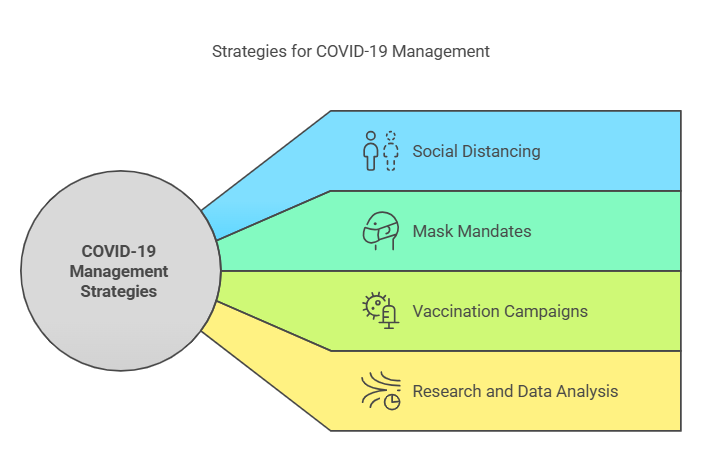
- Key Definitions:
-
Epidemic: A sudden increase in the number of cases of a
disease above what is normally expected in a specific area.
-
Public Health Intervention: Actions taken to prevent
disease, promote health, and prolong life among populations.
- Key Principles:
-
Surveillance: Continuous monitoring of disease spread to
inform public health responses.
-
Containment: Implementing measures such as quarantine and
isolation to prevent further transmission.
-
Vaccination: Promoting and administering vaccines to
achieve herd immunity.
- Relevance to the PNLE Exam:
-
Understanding the principles of epidemic management is crucial, as
questions may focus on the role of nurses in public health crises,
including vaccination strategies and community education.
- Common Misconceptions:
-
Many believe that only public health officials are responsible for
epidemic management; however, nurses play a vital role in education,
vaccination, and community support.
- Practice Question:
-
Which of the following is NOT a key principle of epidemic
management?
- A) Surveillance
- B) Containment
- C) Ignoring the outbreak
- D) Vaccination
Correct Answer:
C) Ignoring the outbreak
Rationale: Ignoring an outbreak contradicts the principles of
epidemic management, which focus on proactive measures.
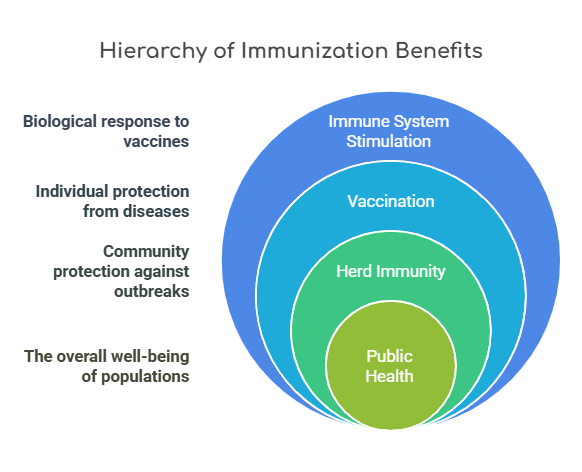
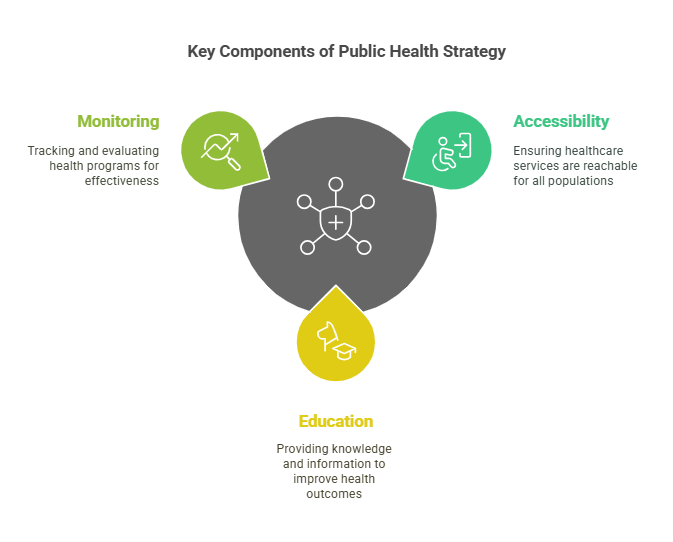
12.2 Immunization Programs
-
Overview: This section covers the importance of
immunization programs in preventing infectious diseases and promoting
community health.
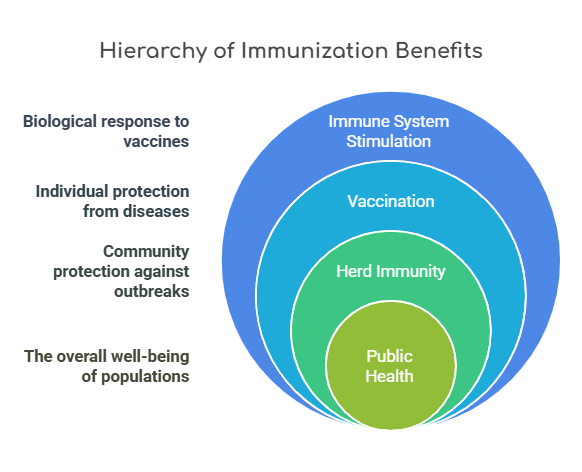
- Key Definitions:
-
Immunization: The process by which an individual’s immune
system becomes fortified against an agent (pathogen).
-
Herd Immunity: When a significant portion of a population
becomes immune to a disease, reducing its spread.
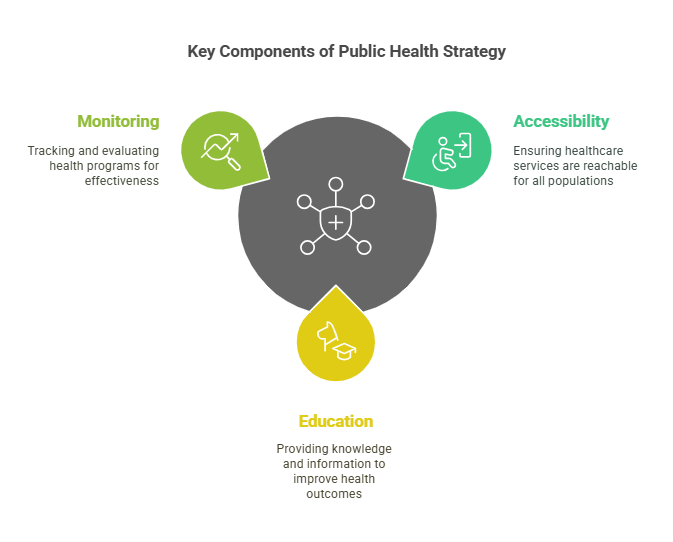
- Key Principles:
-
Accessibility: Ensuring vaccines are available to all
segments of the population.
-
Education: Informing communities about the benefits and
safety of vaccines.
-
Monitoring: Tracking vaccination rates and disease
outbreaks to adapt strategies accordingly.
- Relevance to the PNLE Exam:
-
Questions may address the nurse’s role in immunization, including patient
education and managing vaccine side effects.
- Quick Tips:
-
Remember the acronym AEM for Immunization Programs:
Accessibility, Education,
Monitoring.
-
What is the primary goal of immunization programs?
- A) To eliminate all diseases
- B) To prevent the spread of infectious diseases
- C) To increase healthcare costs
- D) To provide free healthcare
Correct Answer:
B) To prevent the spread
of infectious diseases
Rationale: Immunization programs
aim to reduce the incidence of infectious diseases through widespread
vaccination.
Final Summary
This study guide encapsulates the critical components of NCM 102, focusing on
epidemic management and immunization programs as essential public health
interventions. It prepares nursing students for the PNLE by emphasizing the
importance of proactive health measures and community education. For further
resources and online review materials, please visit our website to enhance your
preparation journey.
Take-Home Message: Nurses are pivotal in public health
interventions, particularly in managing epidemics and promoting immunization to
safeguard community health.




 Key Definitions:
Key Definitions:
 Key Definitions :
Key Definitions :