1. DOH Programs Related to Family Health
Introduction
This chapter focuses on the Department of Health (DOH) programs that address
common conditions detected in family health. Understanding these conditions is
crucial for nursing graduates preparing for the PNLE, as they encompass vital
aspects of maternal and child healthcare.
Key Definitions
Congenital Disorders: Conditions present at birth that can affect health and
development.
- Neonatal: Referring to the first 28 days of life.
- Screening: The process of identifying healthy individuals
who may be at increased risk of a disease or condition.

Key Principles
- Early detection and management of congenital and neonatal conditions can
significantly improve health outcomes. - Nursing interventions play a critical role in the ongoing care and support
for affected families.
1.1. Common Conditions Detected
1.1.1. Congenital Hypothyroidism
- Causes: Genetic factors, maternal iodine deficiency.
- Diagnosis Methods: Newborn screening tests, serum
thyroid-stimulating hormone (TSH) levels. - Signs and Symptoms: Poor feeding, lethargy, hypotonia.
- Treatment: Lifelong thyroid hormone replacement therapy.

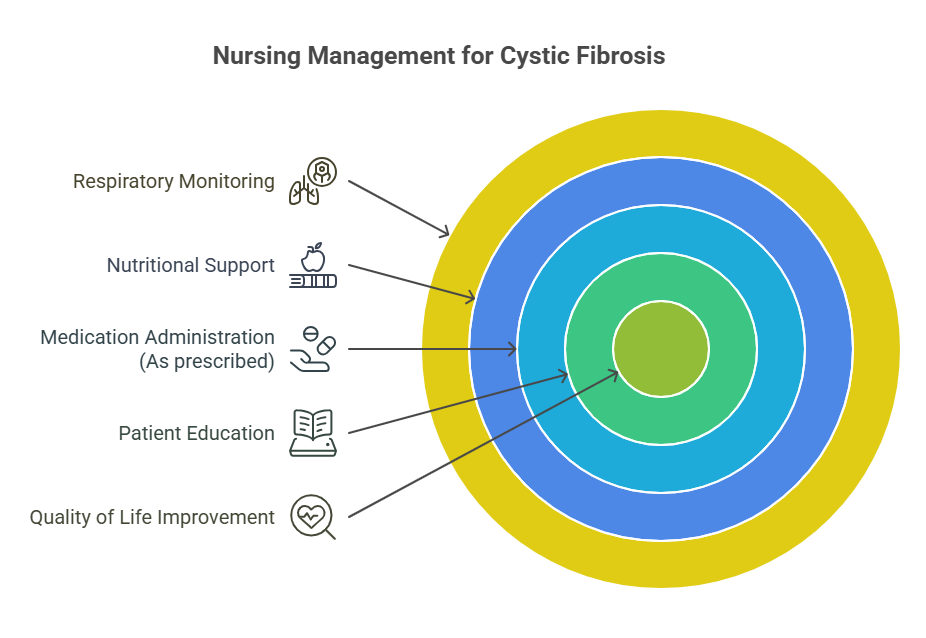
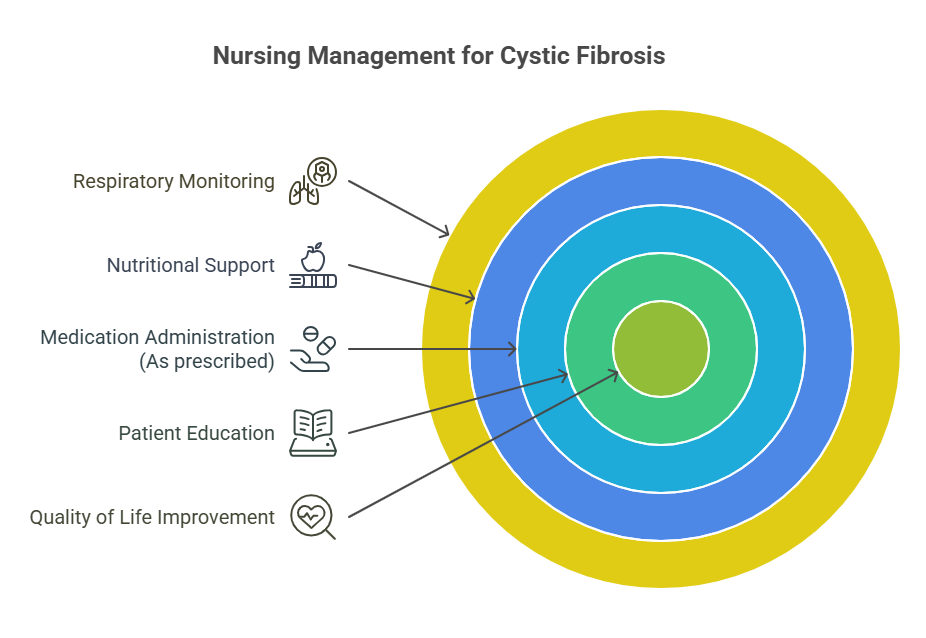
1.1.2. Cystic Fibrosis
- Causes: Genetic mutation in the CFTR gene.
- Diagnostic Tests: Sweat test, genetic testing.
- Management: Airway clearance techniques, enzyme replacement.
- Symptoms: Chronic cough, frequent lung infections, digestive issues.
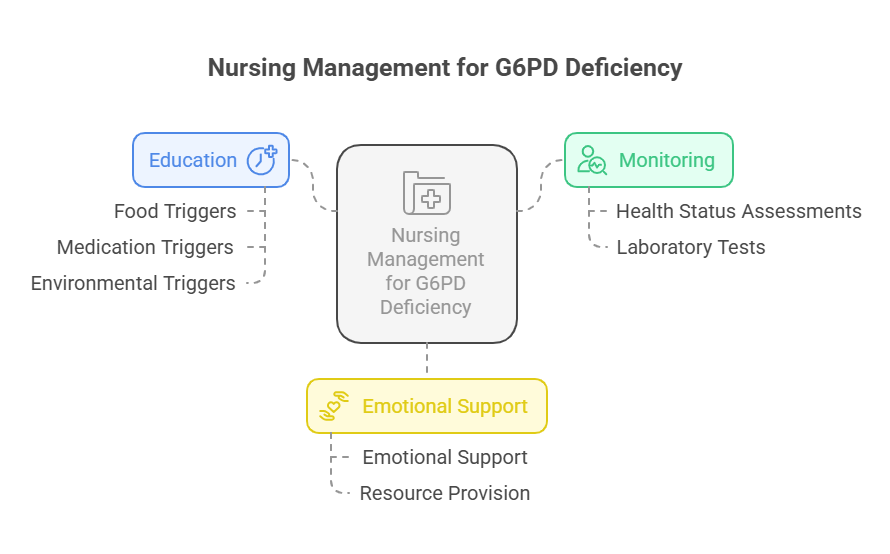
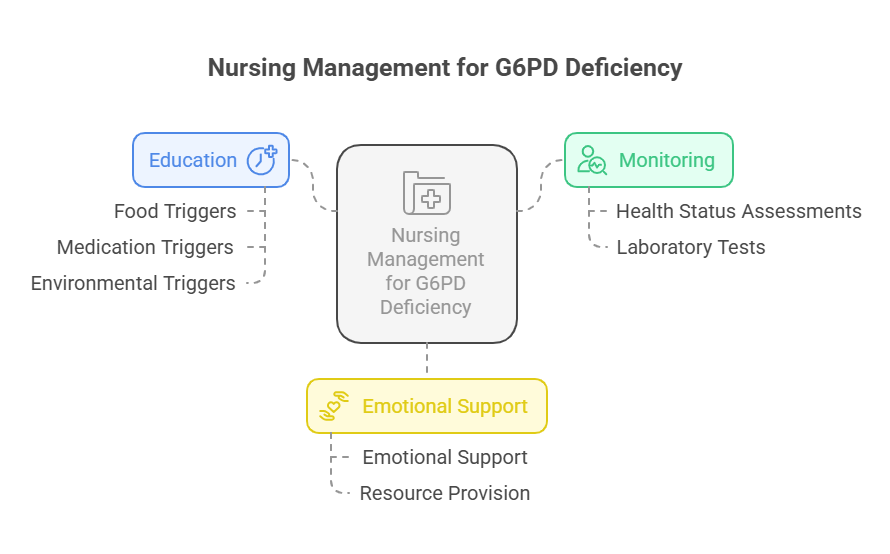
1.1.3. G6PD Deficiency
- Causes: Inherited genetic disorder.
- Management: Avoidance of triggers (certain foods, medications).
- Symptoms: Jaundice, fatigue, dark urine.
- Triggers: Fava beans, certain infections.
1.1.4. Galactosemia
- Causes: Genetic mutation affecting galactose metabolism.
- Diagnosis: Newborn screening, blood tests.
- Management: Lactose-free diet.
- Symptoms: Vomiting, diarrhea, liver damage.

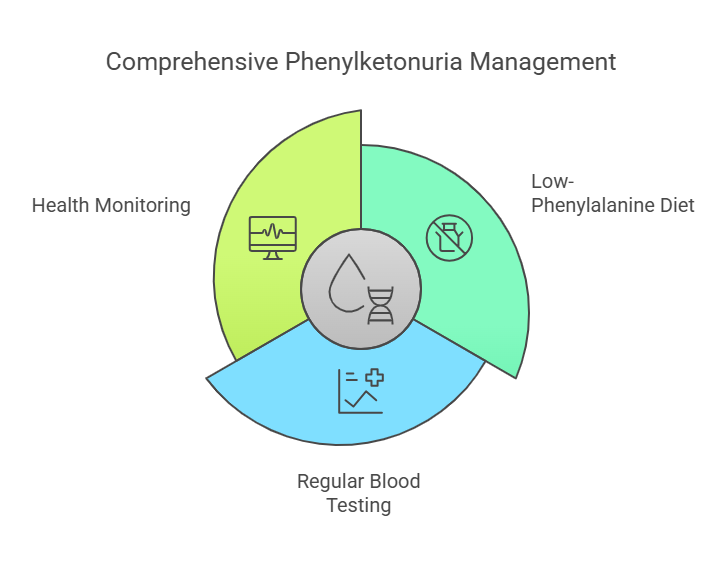
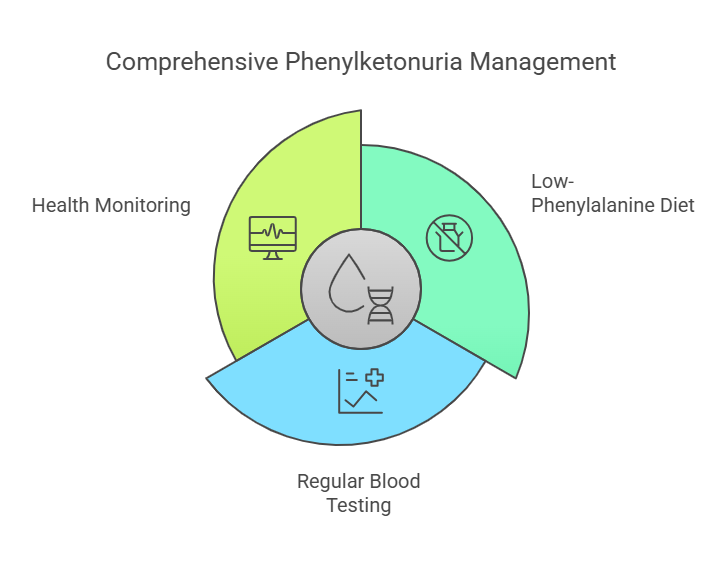
1.1.5. Phenylketonuria (PKU)
- Causes: Genetic mutation affecting phenylalanine metabolism.
- Diagnostic Methods: Newborn screening, blood tests.
- Symptoms: Developmental delays, intellectual disability.
- Treatment: Special diet low in phenylalanine.
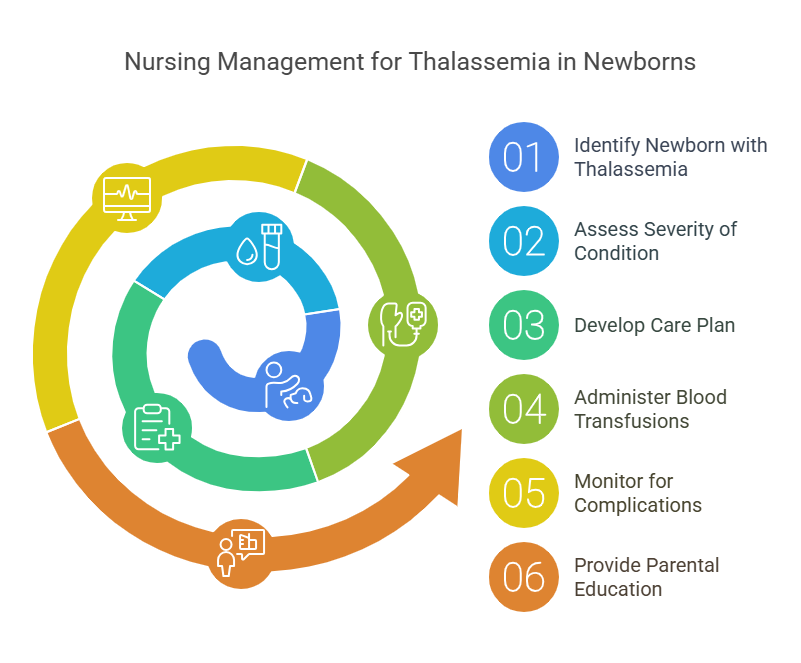
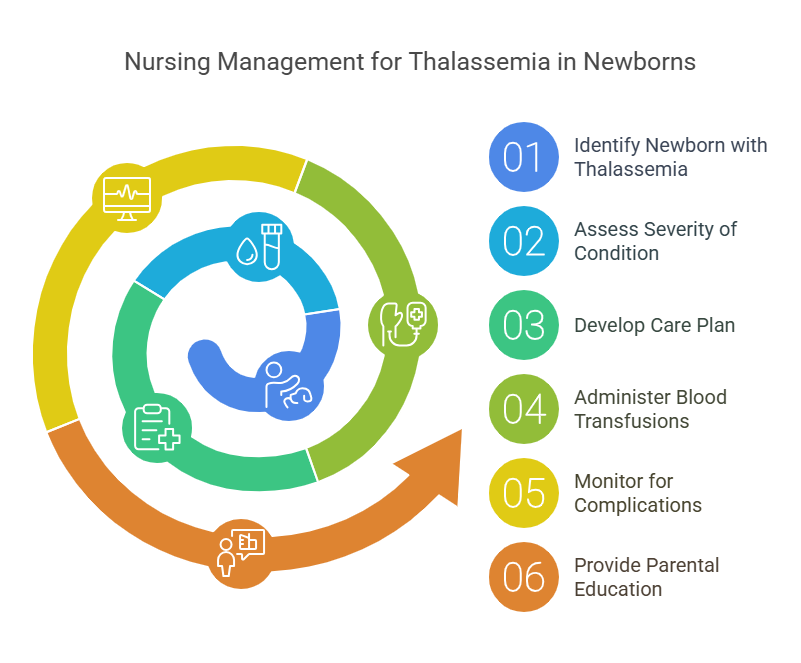
1.1.6. Thalassemia
- Causes: Genetic mutations affecting hemoglobin production.
- Symptoms: Anemia, fatigue, jaundice.
- Screening: Blood tests for hemoglobin levels.
- Nursing Interventions: Education on blood transfusions and iron chelation
therapy.
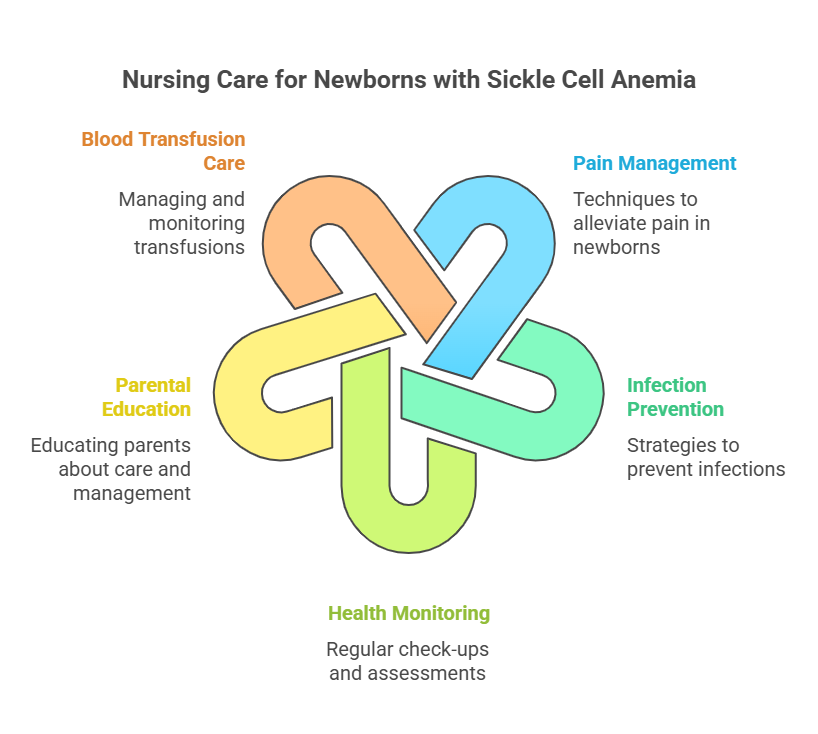
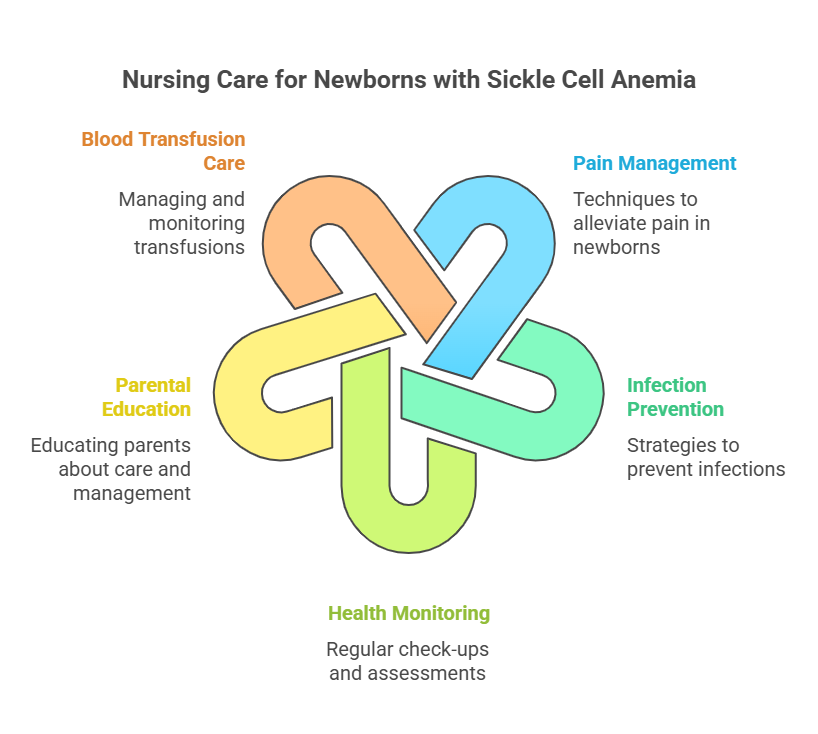
1.1.7. Sickle Cell Anemia
- Causes: Genetic mutation in hemoglobin.
- Symptoms: Pain crises, anemia, increased infections.
- Screening: Newborn screening, hemoglobin electrophoresis.
- Nursing Interventions: Pain management, hydration, education on infection
prevention.
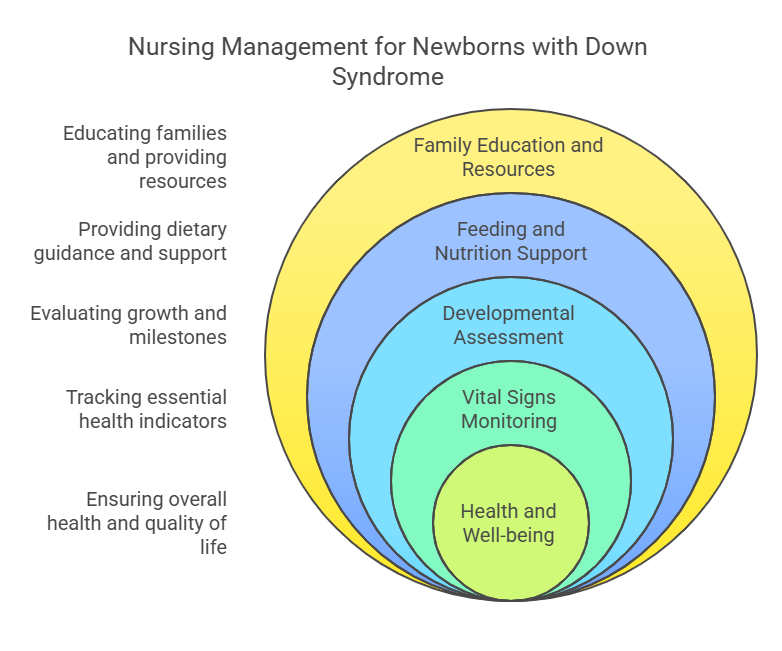
1.1.8. Down Syndrome
- Causes: Chromosomal abnormality (trisomy 21).
- Symptoms: Distinctive facial features, developmental delays.
- Screening: Prenatal screening, genetic testing.
- Nursing Interventions: Early intervention programs, support for families
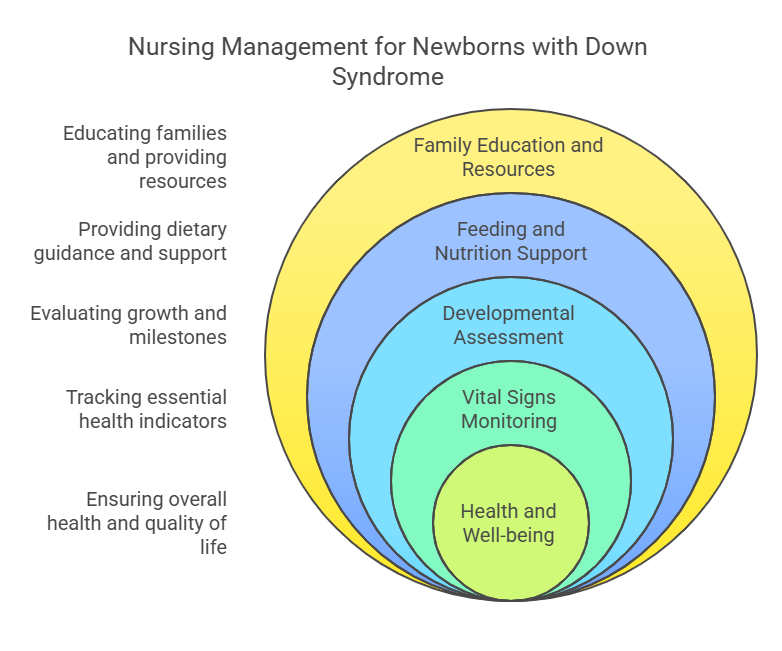
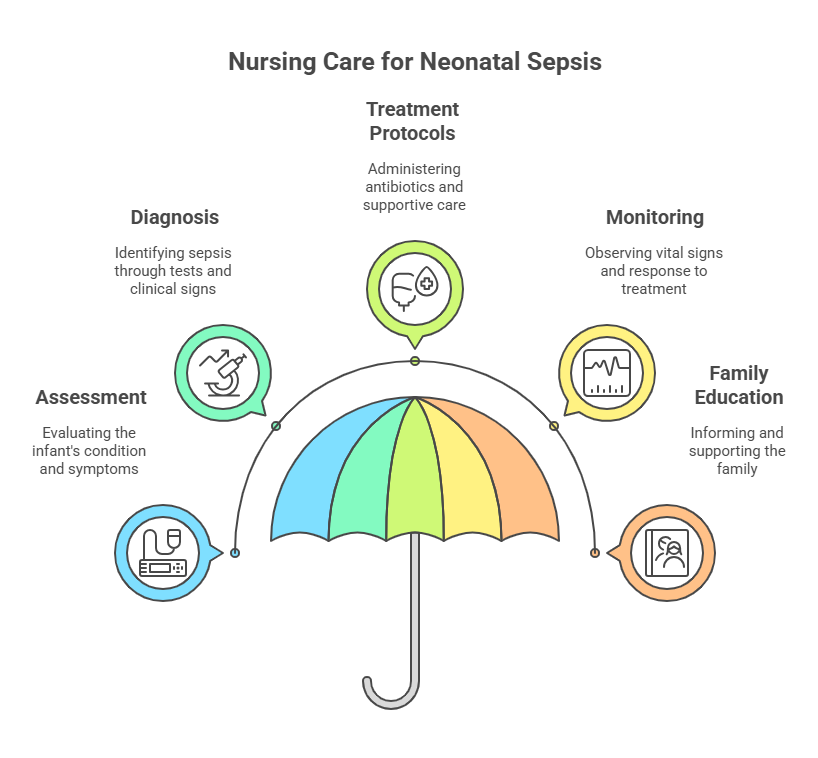
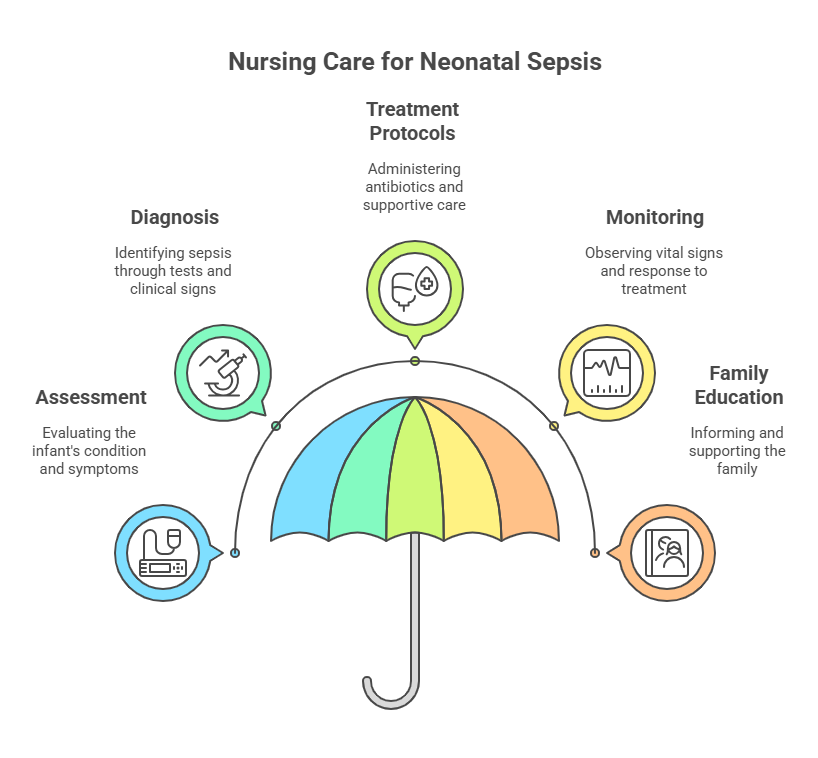
1.1.9. Neonatal Sepsis
- Causes: Bacterial infection during or after birth.
- Symptoms: Temperature instability, poor feeding, lethargy.
- Screening: Blood cultures, clinical assessment.
- Nursing Interventions: Administration of antibiotics, monitoring vital
signs.
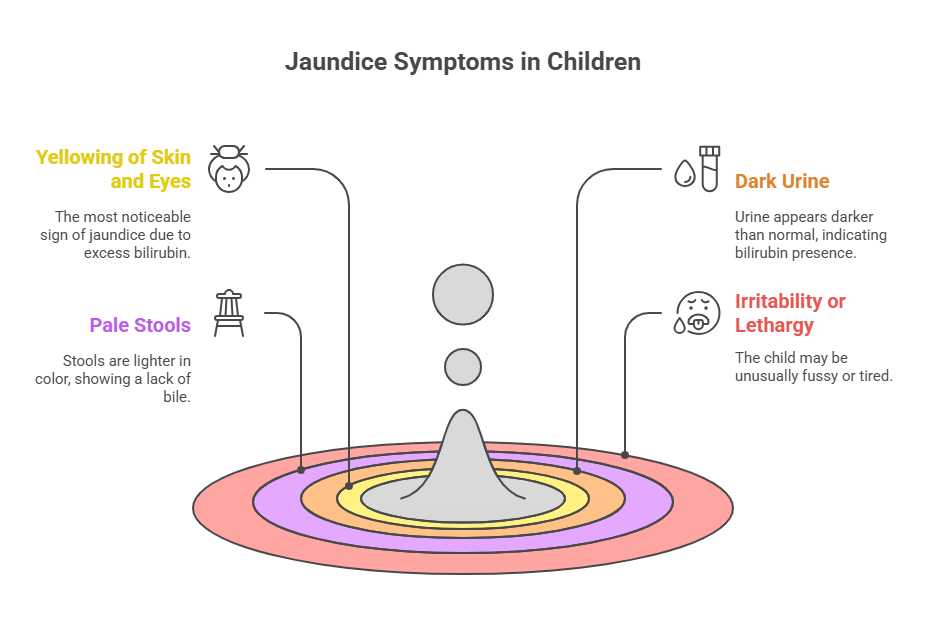
1.1.10. Neonatal Jaundice
- Causes: Immature liver function, hemolysis.
- Symptoms: Yellowing of the skin and eyes.
- Screening: Bilirubin levels, clinical assessment.
- Nursing Interventions: Phototherapy, hydration.

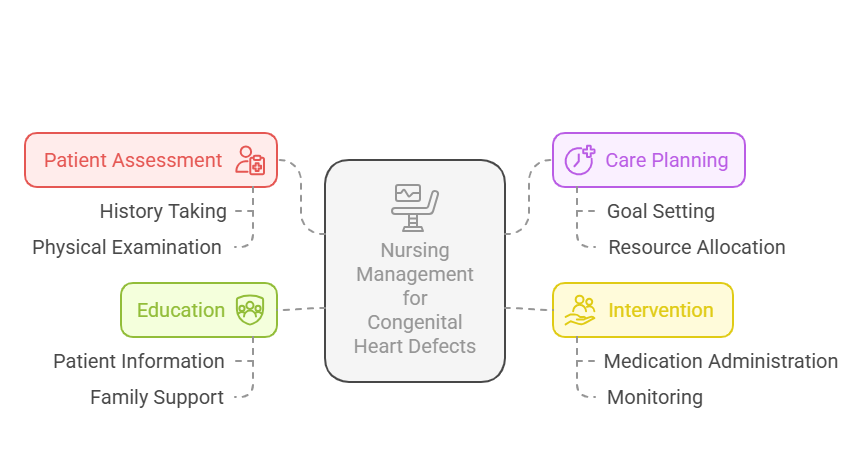
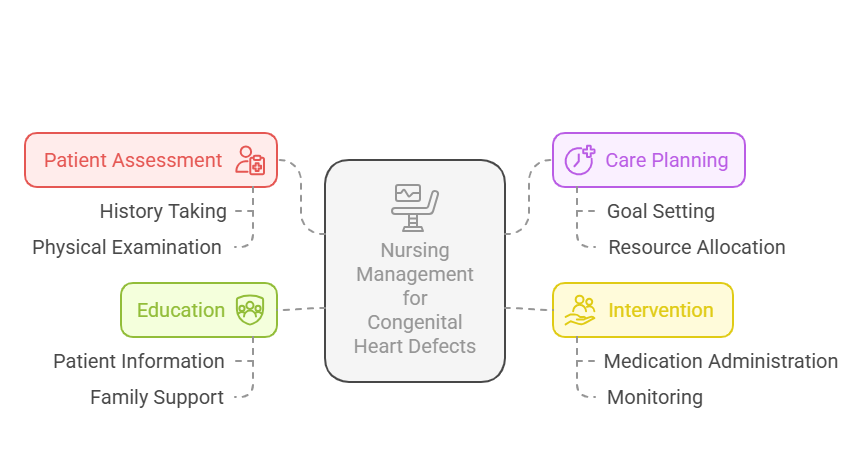
1.1.11. Congenital Heart Defects
- Causes: Genetic and environmental factors.
- Symptoms: Cyanosis, difficulty breathing, poor feeding.
- Screening: Pulse oximetry, echocardiogram.
- Nursing Interventions: Education on care and potential surgical
interventions.
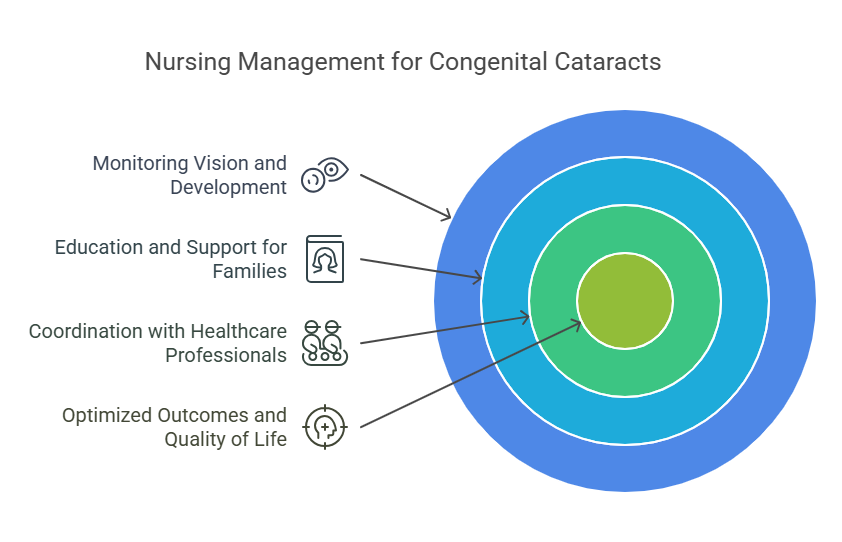
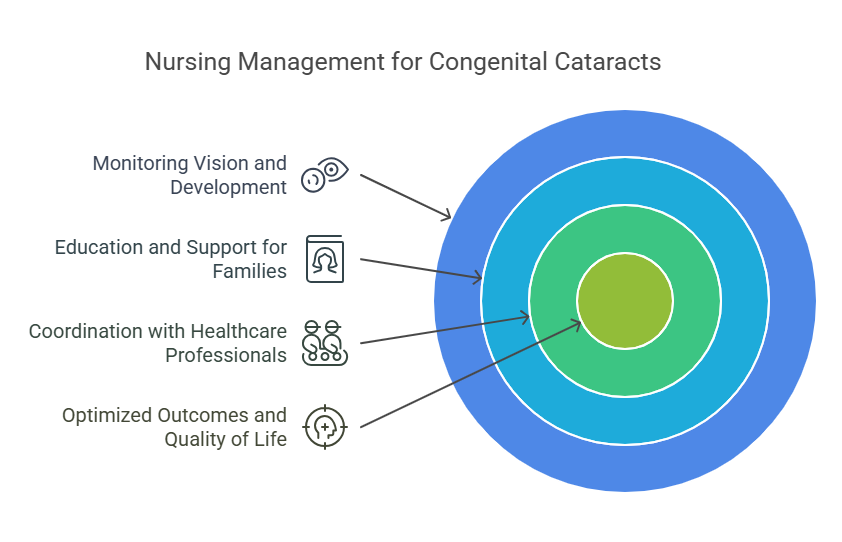
1.1.12. Congenital Cataracts
- Causes: Genetic factors, maternal infections.
- Symptoms: Cloudy appearance of the lens, vision problems.
- Screening: Eye examination.
- Nursing Interventions: Referral for surgical intervention, family education.
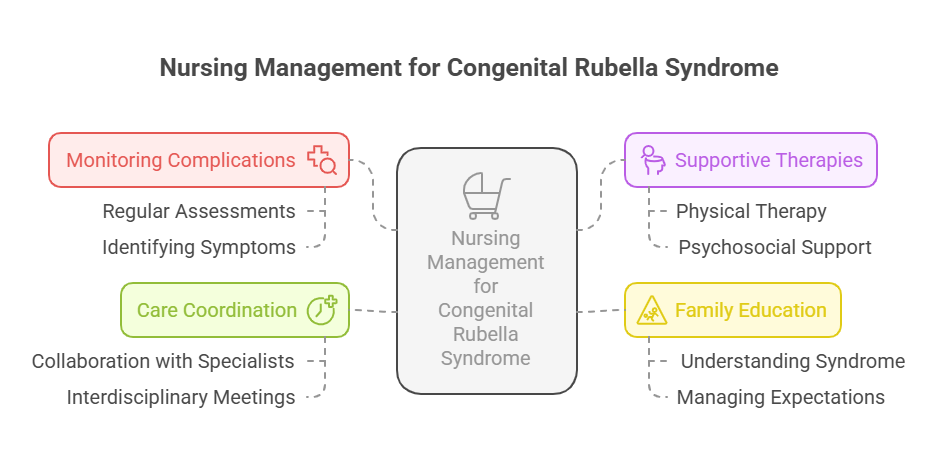
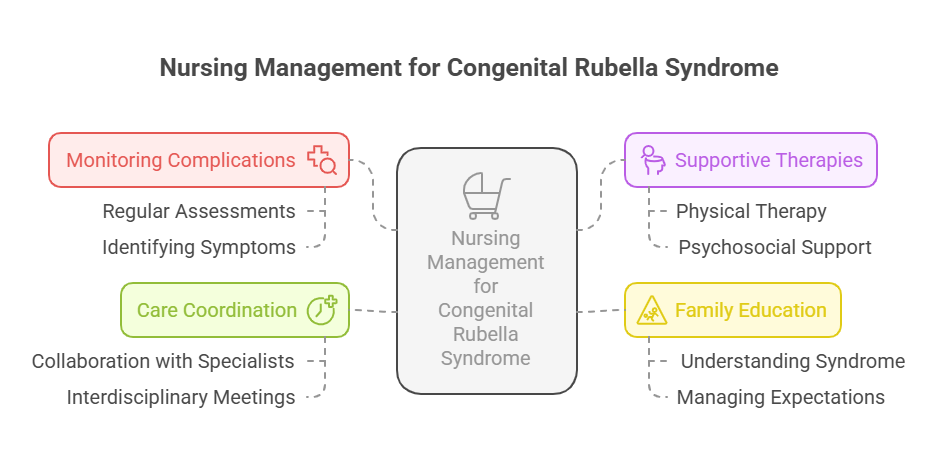
1.1.13. Congenital Rubella Syndrome
- Causes: Maternal rubella infection during pregnancy.
- Symptoms: Hearing loss, heart defects, developmental delays.
- Screening: Serological tests for rubella immunity.
- Nursing Interventions: Supportive care, early intervention services.
1.1.14. Neonatal Hypoglycemia
- Causes: Maternal diabetes, prematurity.
- Symptoms: Jitteriness, poor feeding, lethargy.
- Screening: Blood glucose levels.
- Nursing Interventions: Feeding, glucose administration as needed.

Relevance to the PNLE Exam
- Familiarity with these conditions is critical as they are often included in
PNLE exam questions related to maternal and child health. - Understanding the nursing interventions for each condition is essential for
clinical practice scenarios.
Practice Questions
- Which of the following is a common symptom of congenital hypothyroidism?
- A) Jaundice
- B) Poor feeding
- C) Cyanosis
- D) Cloudy lens
Correct Answer: B) Poor feeding. Rationale: Poor feeding is a key symptom
indicating potential congenital hypothyroidism.
- What is the primary management for G6PD deficiency?
- A) Blood transfusions
- B) Avoidance of triggers
- C) Antibiotic therapy
- D) Phototherapy
Correct Answer: B) Avoidance of triggers. Rationale: Management involves
avoiding substances that can trigger hemolysis.
Take-Home Message
Early detection and effective management of common congenital and neonatal
conditions are essential for improving health outcomes in family health
programs.”
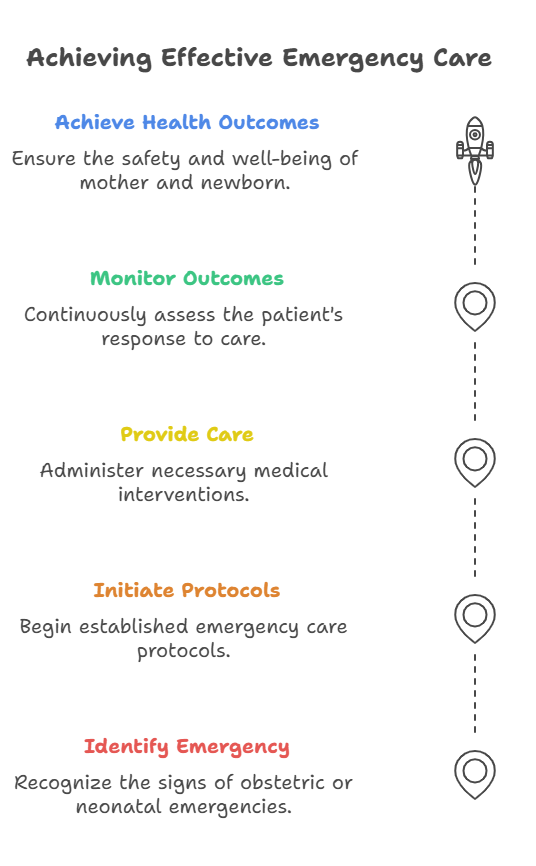
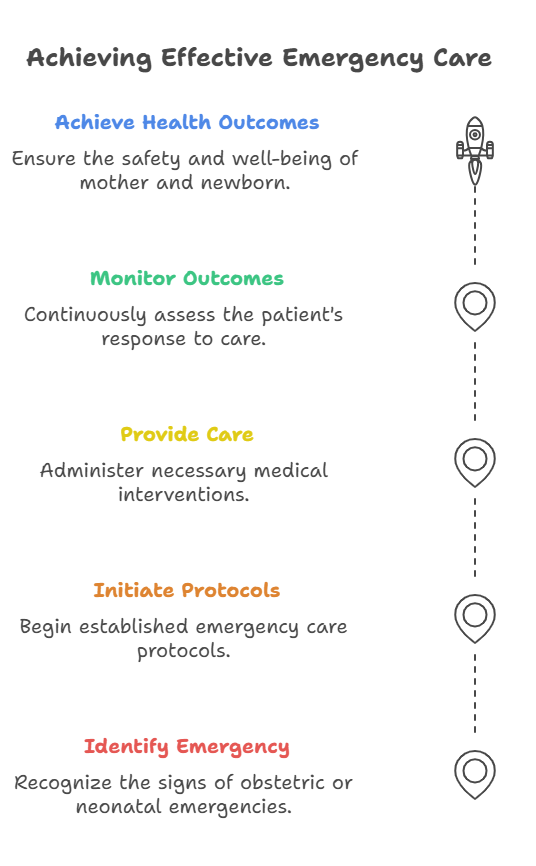
2. Components of BEmONC
General Introduction
This section outlines the Basic Emergency Obstetric and Newborn Care (BEmONC)
components essential for managing maternal and neonatal health emergencies.
Understanding these components is crucial for nursing graduates preparing for
the PNLE, as they encompass critical interventions necessary for safe childbirth
and maternal care.
Key Definitions
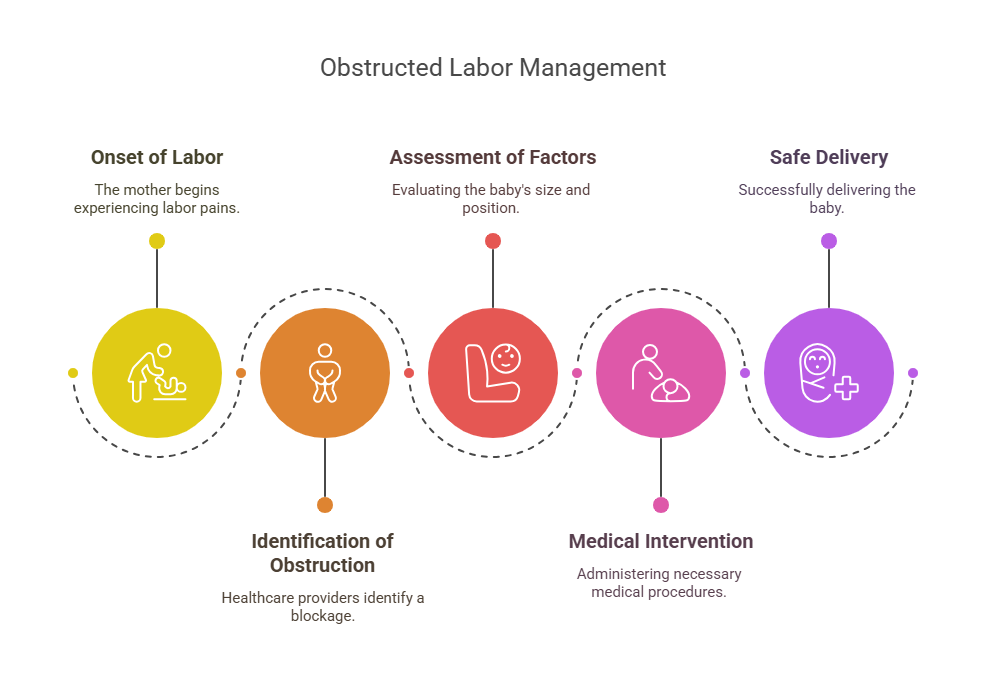
- BEmONC: A set of lifesaving interventions for managing complications during
pregnancy, childbirth, and the postpartum period. - Obstructed Labor: A condition where the baby cannot progress through the
birth canal due to various factors.
- Postpartum Hemorrhage (PPH): Excessive bleeding following childbirth, which
can be life-threatening.
Key Principles
- Timely and effective intervention can prevent maternal and neonatal
morbidity and mortality. - Health promotion through routine practices, such as vaccination, is
essential for maternal and child health. - Understanding the signs and symptoms of complications enables prompt
management.
2.1. Emergency Obstetric Care
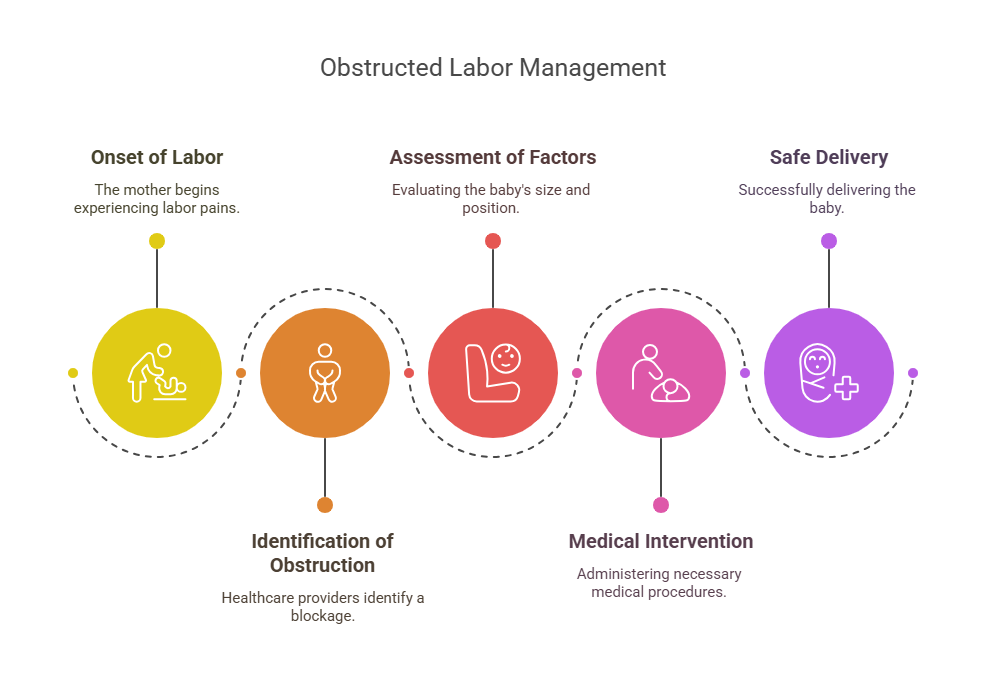
2.1.1. Management of Obstructed Labor
- Key Points:
- Recognize signs of obstructed labor (e.g., prolonged labor).
- Interventions may include manual rotation or cesarean delivery if
necessary.
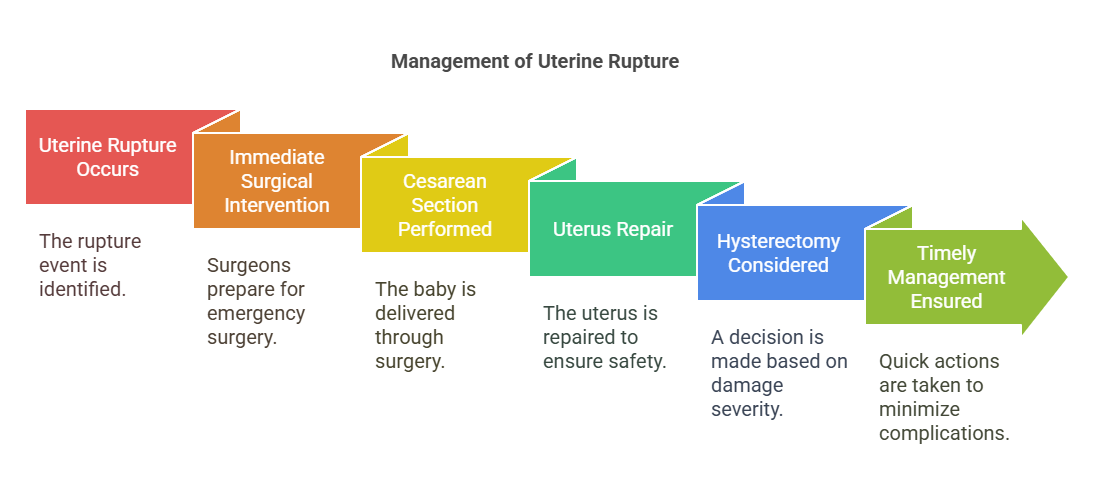
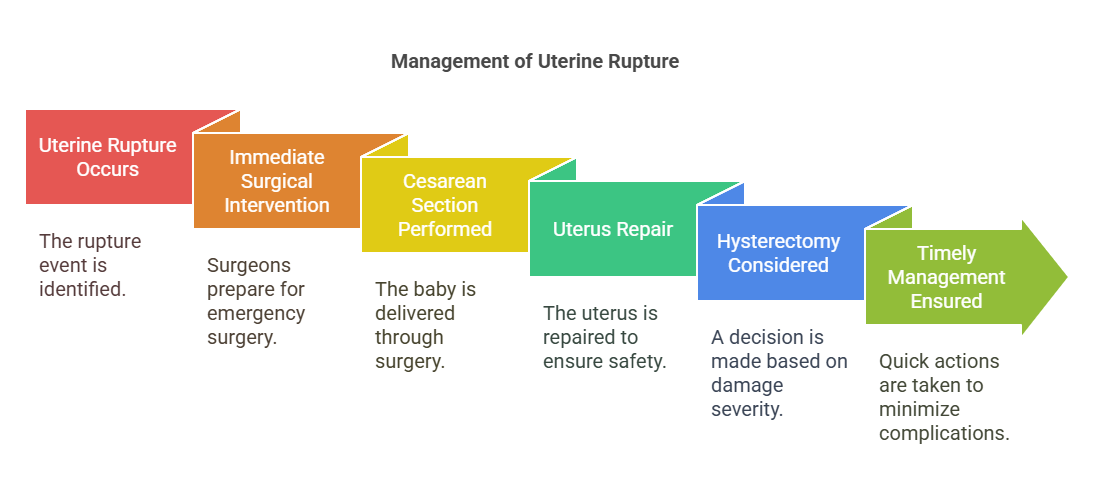
2.1.2. Treatment of Uterine Rupture
- Key Points:
- Uterine rupture can lead to severe hemorrhage and requires immediate
surgical intervention. - Signs include sudden abdominal pain and fetal distress.
2.2. Health Promotion
2.2.1. Routine Vaccination
- Key Points:
- Vaccination protects mothers and infants from preventable diseases.
- Essential vaccines include Tetanus Toxoid and Influenza.
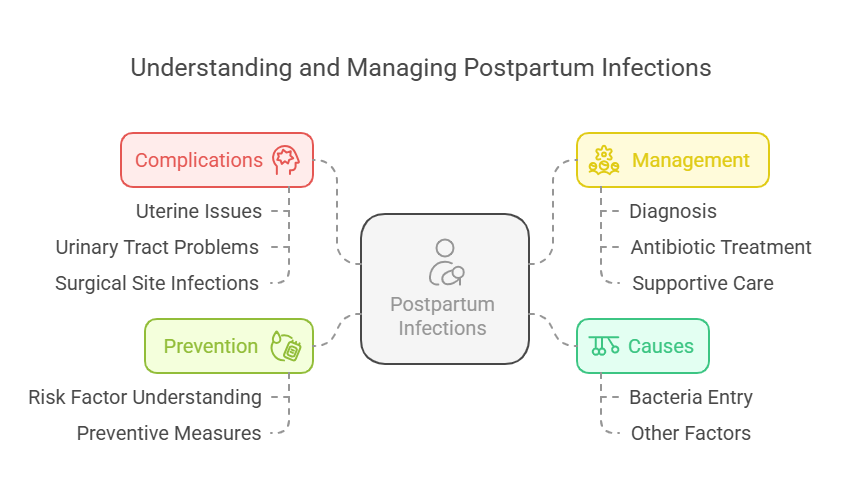
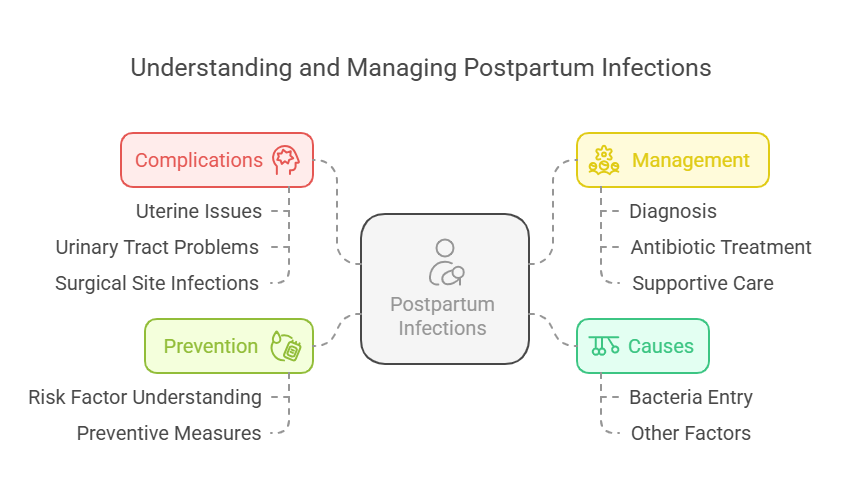
2.3. Management of Postpartum Infections
2.3.1. Causes
- Key Points:
- Common causes include retained placental fragments and poor hygiene.
2.3.2. Interventions
- Key Points:
- Administer antibiotics and ensure proper wound care.
2.3.3. Signs and Symptoms
- Key Points:
- Fever, foul-smelling discharge, and abdominal pain indicate infection.
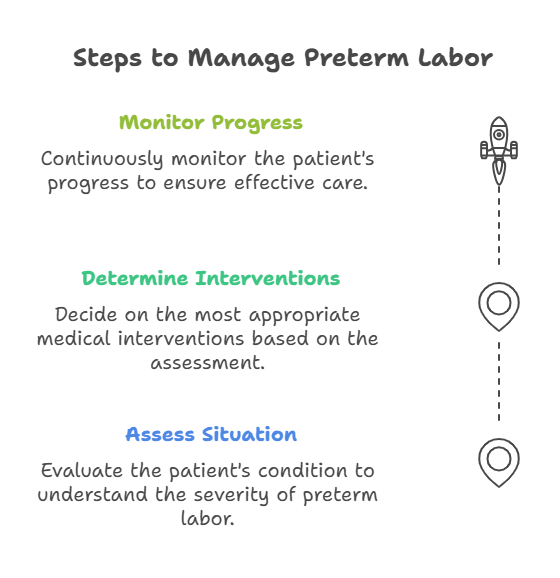
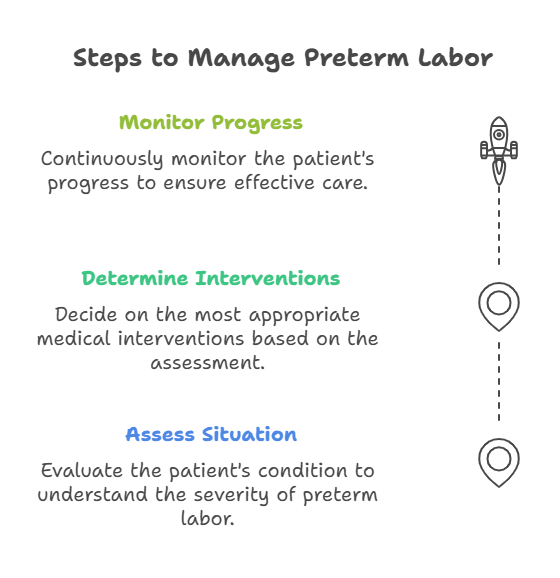
2.4. Management of Preterm Labor
2.4.1. Interventions
- Key Points:
- Administer tocolytics to delay labor and corticosteroids for fetal lung
maturity.
2.4.2. Risk Factors
- Key Points:
- Include history of preterm birth, multiple pregnancies, and infections.
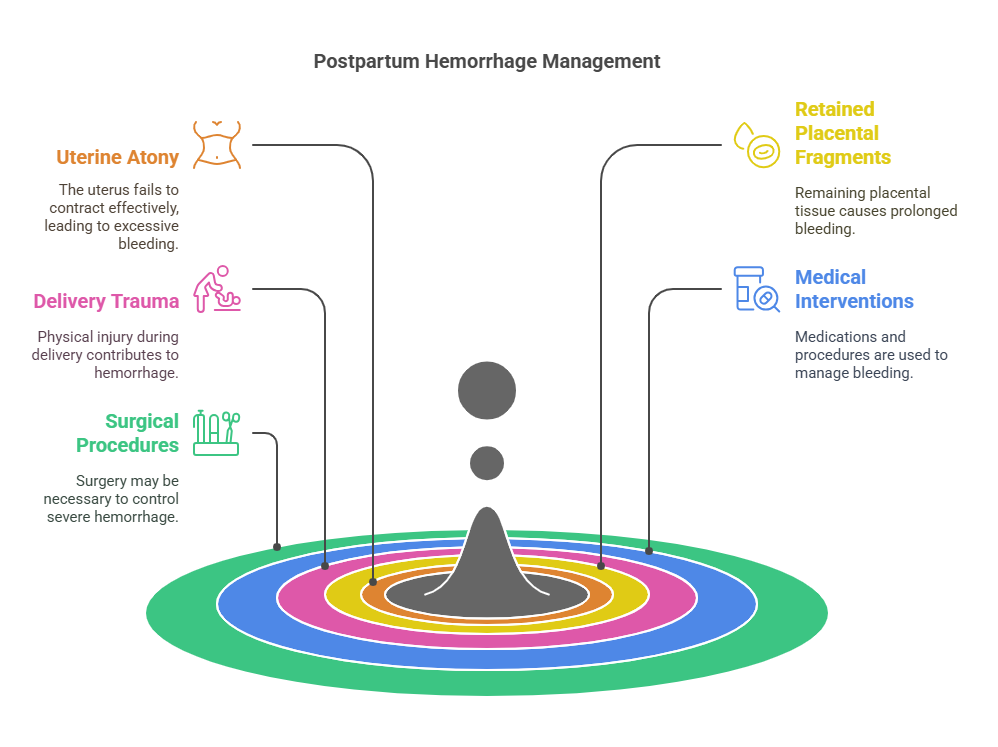
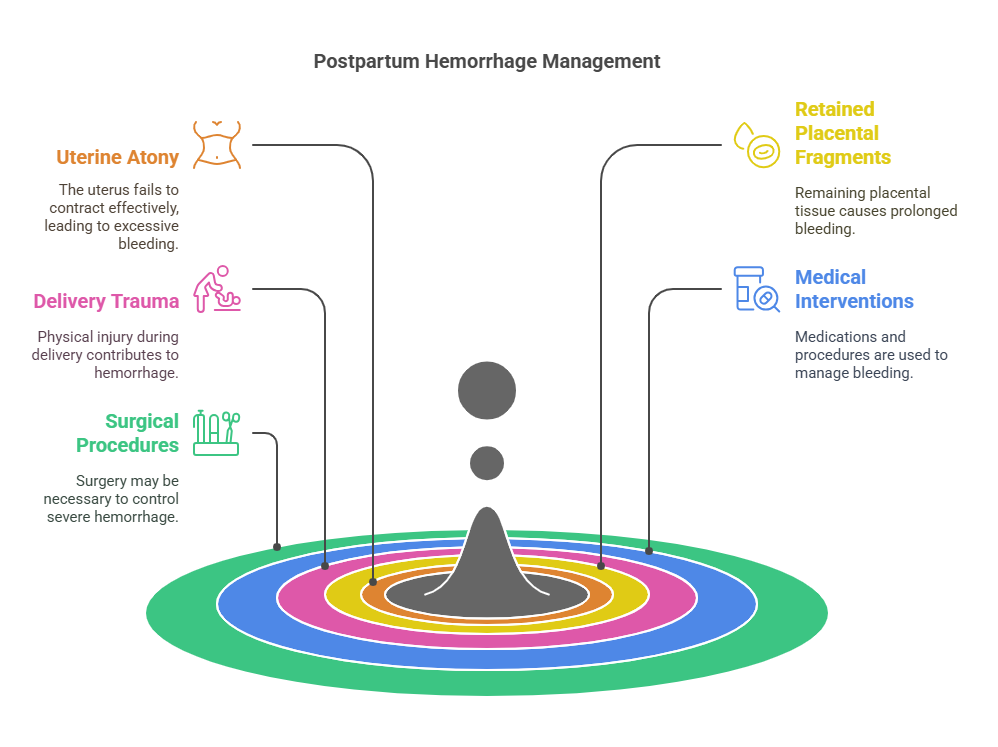
2.5. Managing Postpartum Hemorrhage
2.5.1. Causes and Risk Factors
- Key Points:
- Causes include uterine atony, retained placenta, and trauma during
delivery.
2.5.2. Interventions
- Key Points:
- Fundal massage, administration of uterotonics, and fluid resuscitation.
2.5.3. Signs and Symptoms
- Key Points:
- Heavy vaginal bleeding, hypotension, and tachycardia.
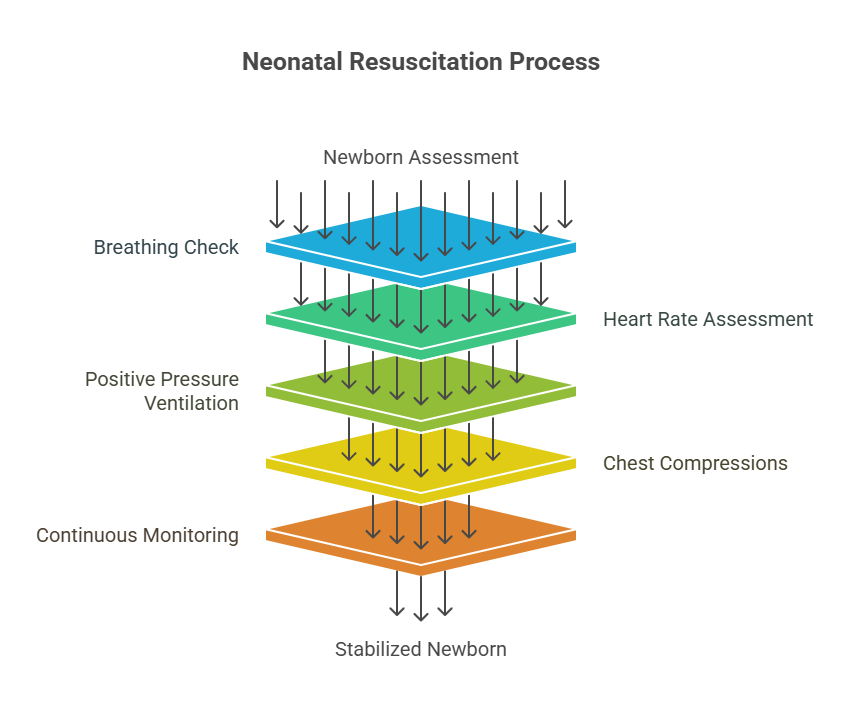
2.6. Neonatal Resuscitation
2.6.1. Initial Steps
- Key Points:
- Assess airway, breathing, and circulation immediately after birth.
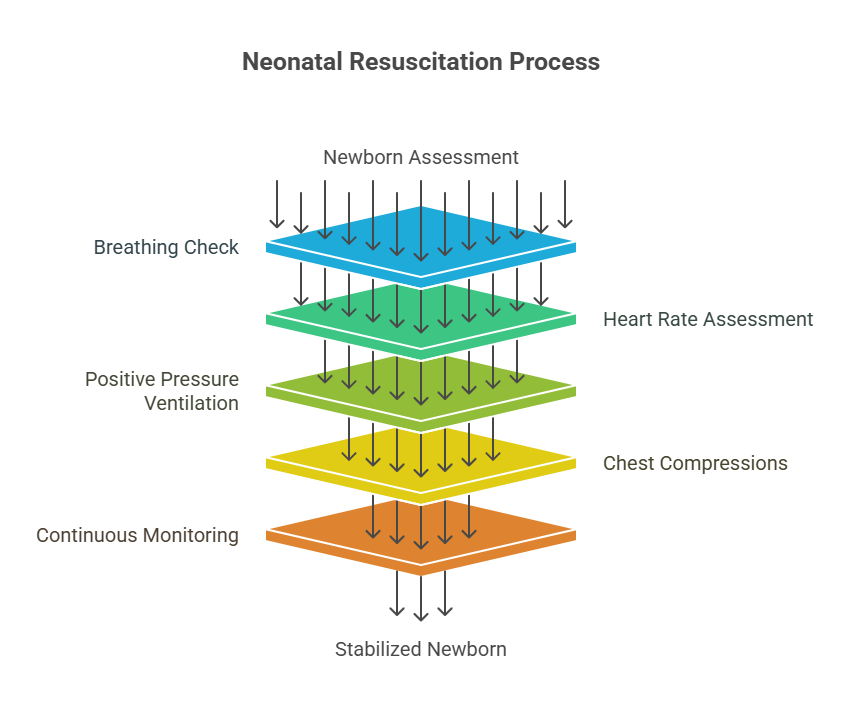
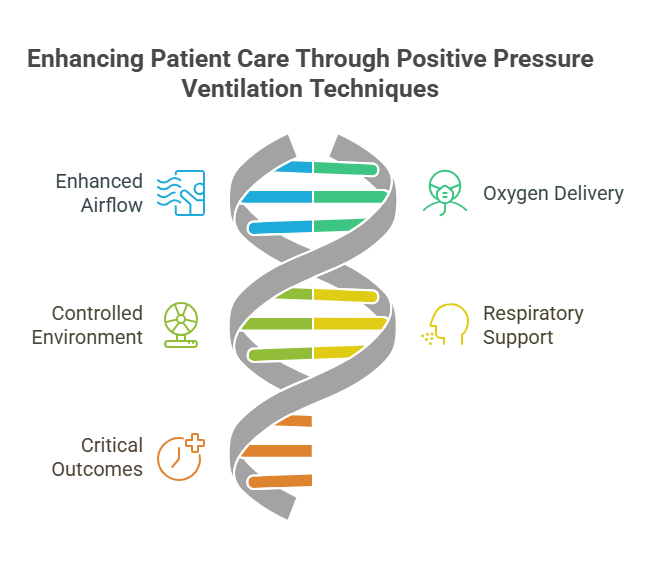
2.6.2. Positive Pressure Ventilation (PPV)
- Key Points:
- Administer PPV if the newborn is not breathing adequately.
Relevance to the PNLE Exam
- Expect questions on the identification and management of obstetric
emergencies, particularly regarding postpartum hemorrhage and neonatal
resuscitation.
Practice Questions
- Which of the following is a common cause of postpartum hemorrhage?
- A) Uterine atony
- B) Preterm labor
- C) Routine vaccination
- D) Obstructed labor
Correct Answer: A) Uterine atony Rationale: Uterine atony is the most common
cause of postpartum hemorrhage.
- What is the first step in neonatal resuscitation?
- A) Positive pressure ventilation
- B) Assessing the airway
- C) Administering drugs
- D) Providing warmth
Correct Answer: B) Assessing the airway Rationale: Ensuring a clear airway is
the initial step in neonatal resuscitation.
Common Misconceptions
- Many believe that all postpartum bleeding is normal; however, significant
bleeding should always be investigated for potential complications.
Quick Tips
- Remember the 4 T’s of postpartum hemorrhage: Tone, Trauma, Tissue, and
Thrombin.
Take-Home Message
Effective management of BEmONC components is vital for ensuring the safety and
health of mothers and newborns during emergencies.”
3. Nutrition Programs in the Philippines
Introduction
This section reviews essential nutrition programs in the Philippines, focusing
on micronutrient supplementation, management of severe acute malnutrition, food
fortification, and growth monitoring. Understanding these programs is crucial
for nursing graduates preparing for the PNLE, as they highlight the role of
nurses in promoting community health and addressing nutritional deficiencies.
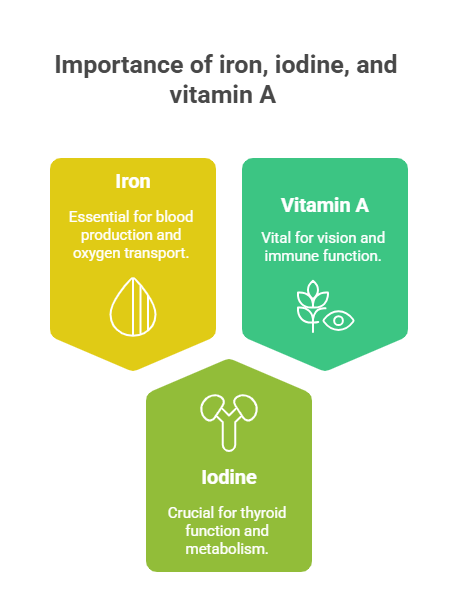
3.1. Micronutrient Supplementation
- Key Definitions:
- Micronutrients: Vitamins and minerals required in small amounts for proper
health. - Supplementation: The process of providing additional nutrients to prevent
deficiencies.
- Key Principles:
- Importance of iron, iodine, and vitamin A in preventing common
deficiencies. - Strategies for effective distribution and education on supplementation.
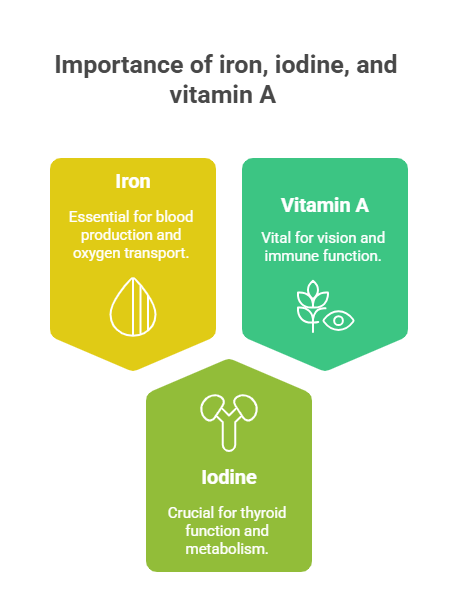
- Relevance to the PNLE Exam:
- Frequently tested on the importance of micronutrients in maternal and
child health.
- Practice Question:
- What is the primary purpose of micronutrient supplementation in children?
- A) To increase appetite
- B) To prevent nutritional deficiencies
- C) To promote weight gain
- D) To enhance physical activity
Correct Answer: B) To prevent nutritional deficiencies. Rationale: Micronutrient
supplementation aims to address and prevent deficiencies that can lead to
serious health issues.
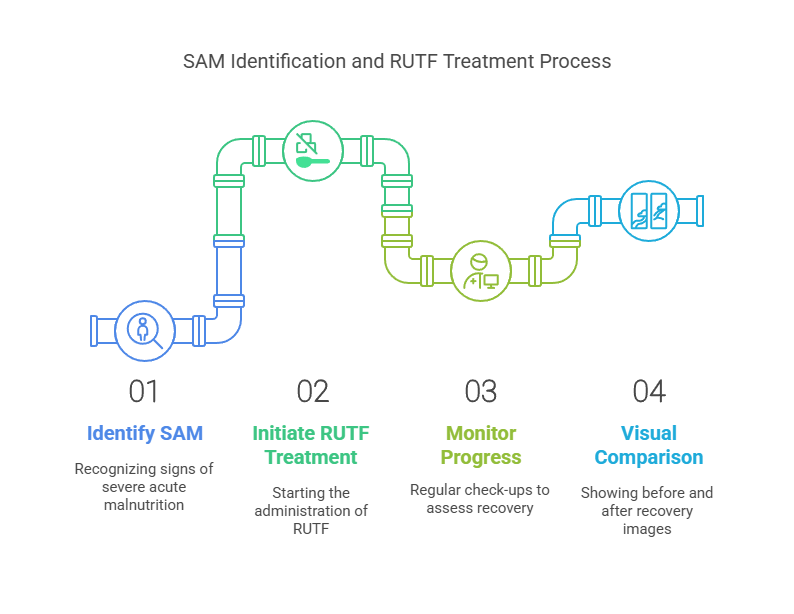
3.2. Addressing Severe Acute Malnutrition
3.2.1. Identification of Malnourished Children
- Key Definitions:
- Severe Acute Malnutrition (SAM): A life-threatening condition
characterized by very low weight for height.
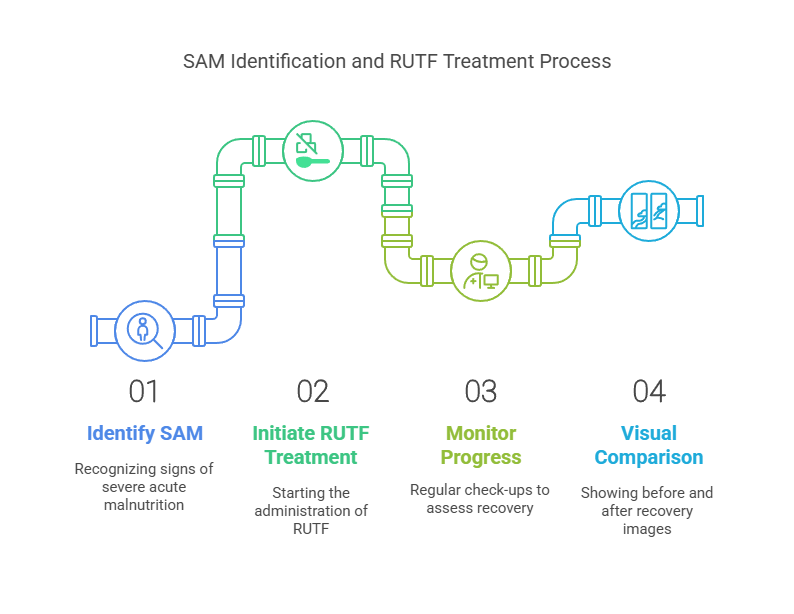
- Key Principles:
- Use of weight-for-height measurements to identify SAM.
- Importance of early detection and intervention.
3.2.2. Monitoring and Follow-ups
- Key Principles:
- Regular follow-up visits to assess recovery and nutritional status.
- Importance of caregiver education on nutrition.
3.2.3. Ready-to-Use Therapeutic Foods (RUTF)
- Key Definitions:
- RUTF: Nutrient-dense food designed for the treatment of SAM.
- Key Principles:
- RUTF provides essential nutrients in a palatable form for children.
- Easy to administer and does not require preparation.
3.2.4. Referral Systems
- Key Principles:
- Establishing clear referral pathways for severe cases to specialized care.
- Collaboration with local health facilities for comprehensive management.
- Common Misconceptions:
- Misunderstanding that malnutrition only refers to undernutrition; it can
also include overnutrition.
3.3. Food Fortification Programs
3.3.1. Iron-Fortified Rice
- Key Definitions:
- Food Fortification: The process of adding essential nutrients to food.
- Key Principles:
- Iron-fortified rice aims to reduce iron deficiency anemia in the
population.
3.3.2. Vitamin A-Fortified Oil
- Key Principles:
- Vitamin A fortification helps combat blindness and immune deficiencies.
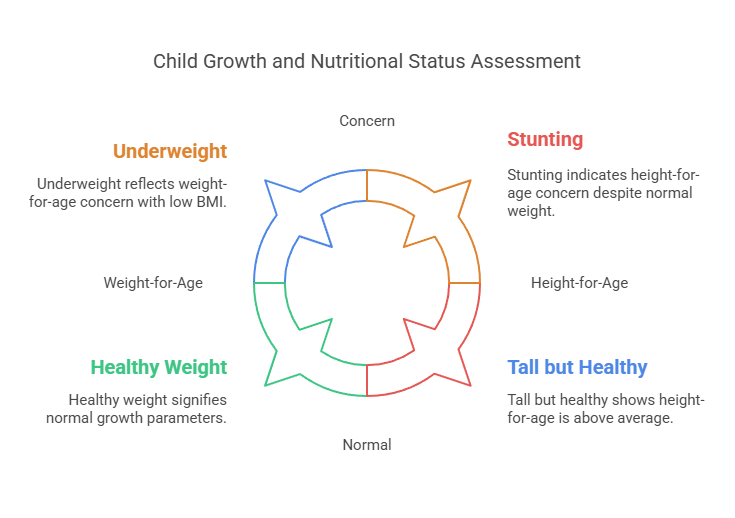
3.4. Growth Monitoring
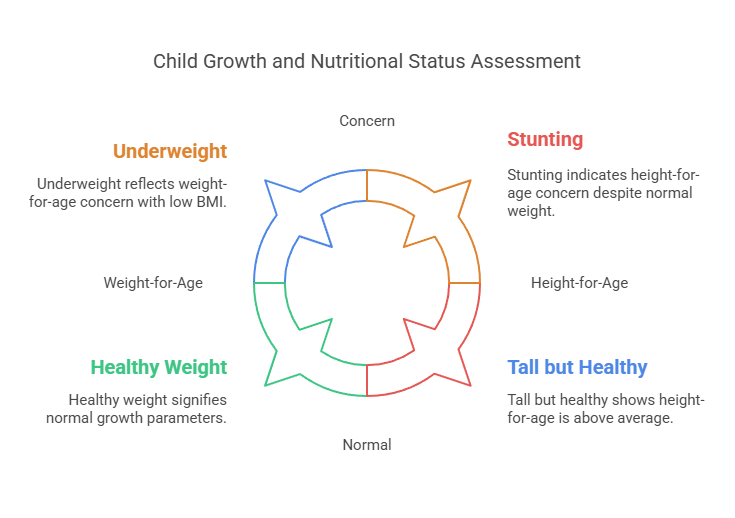
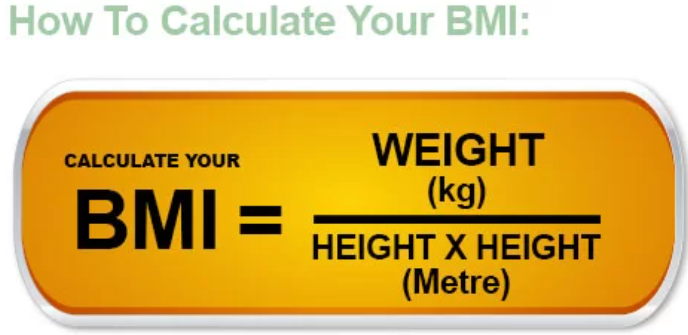
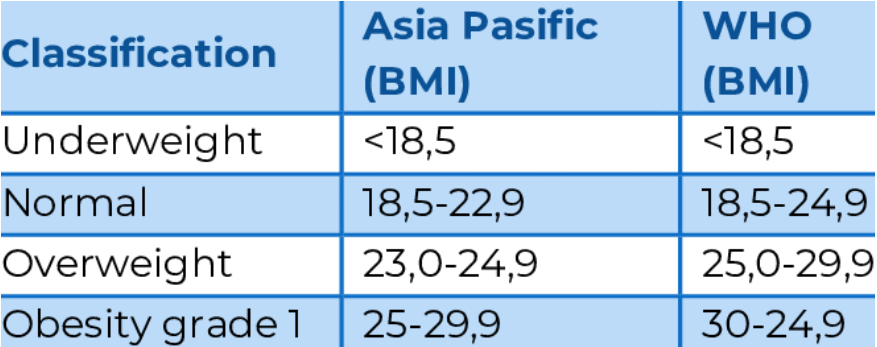
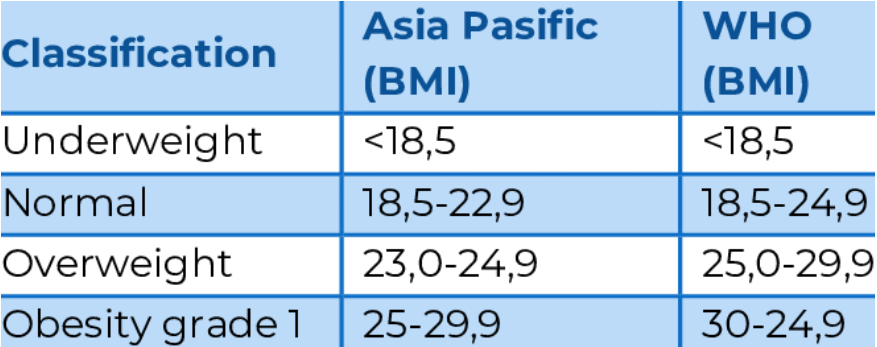
3.4.1. Body Mass Index (BMI) Calculation
- Key Definitions:
- BMI: A measure of body fat based on height and weight.
- Key Principles:
- Regular BMI assessments help identify underweight and overweight children.
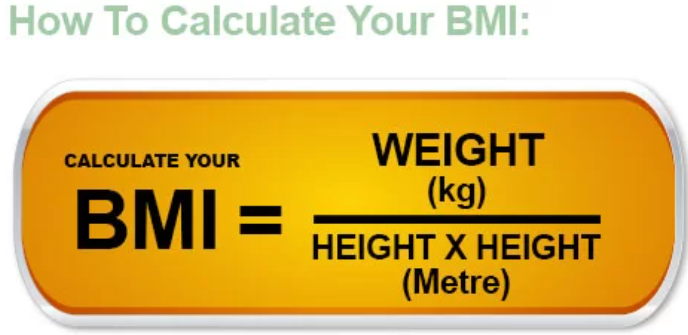
Guidelines based on Asia-Pacific and WHO Obesity guidelines:
3.4.2. Community-Level Growth Campaigns
- Key Principles:
- Engaging communities in growth monitoring encourages awareness and
participation.
3.4.3. Height-for-Age Measurement
- Key Principles:
- Assessing height-for-age helps identify stunting in children.
3.4.4. Regular Weight Monitoring
- Key Principles:
- Consistent weight checks are crucial for tracking growth patterns.
3.4.5. Weight-for-Age Measurement
- Key Principles:
- This measurement helps assess overall health and nutritional status.
Take-Home Message
Effective nutrition programs are vital for preventing malnutrition and promoting
the health of mothers and children in the Philippines, making them essential
knowledge for nursing practice and PNLE preparation.”
4. Integrated Management of Childhood Illnesses (IMCI)
Introduction
This section focuses on the Integrated Management of Childhood Illnesses (IMCI),
a comprehensive approach to improving child health through effective case
management and addressing common childhood conditions. It is crucial for nursing
graduates preparing for the PNLE to understand the IMCI framework, which
emphasizes early detection and management of illnesses in children.
Key Definitions
- Integrated Management of Childhood Illnesses (IMCI): A strategy developed by
the World Health Organization (WHO) to reduce mortality and morbidity in
children under five by improving the way childhood illnesses are managed. - Case Management: A systematic approach to assessing, planning, implementing,
and evaluating the care of a child with a health issue.
Key Principles
- Holistic Approach: IMCI integrates preventive and curative care, focusing on
the child’s overall health and development. - Family and Community Involvement: Engaging families and communities in the
care process enhances the effectiveness of interventions. - Evidence-Based Practices: Utilizing guidelines and protocols based on
research to inform clinical decisions.
4.1. Case Management Process
4.1.1. Classification of Illness Severity
- Key Points: Classifying illness severity helps prioritize treatment and
interventions based on the child’s condition. - Categories:
- Severe: Requires immediate medical attention.
- Non-Severe: Can be managed at home with appropriate guidance.
4.1.2. Initial Assessment of the Child
- Components:
- History taking (symptoms, duration)
- Physical examination (vital signs, general appearance)
- Importance: Accurate assessment is critical for effective management and
treatment.
4.2. Common Childhood Conditions
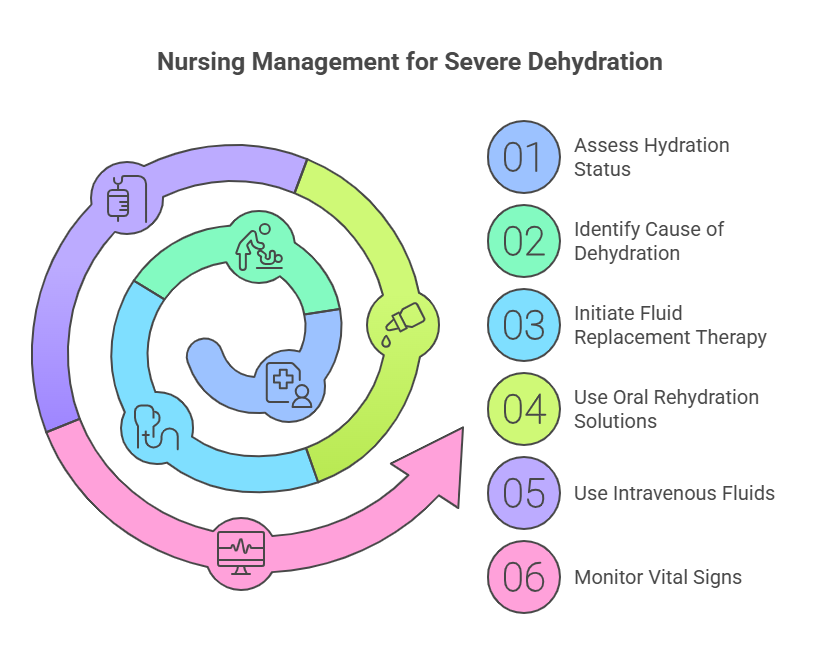
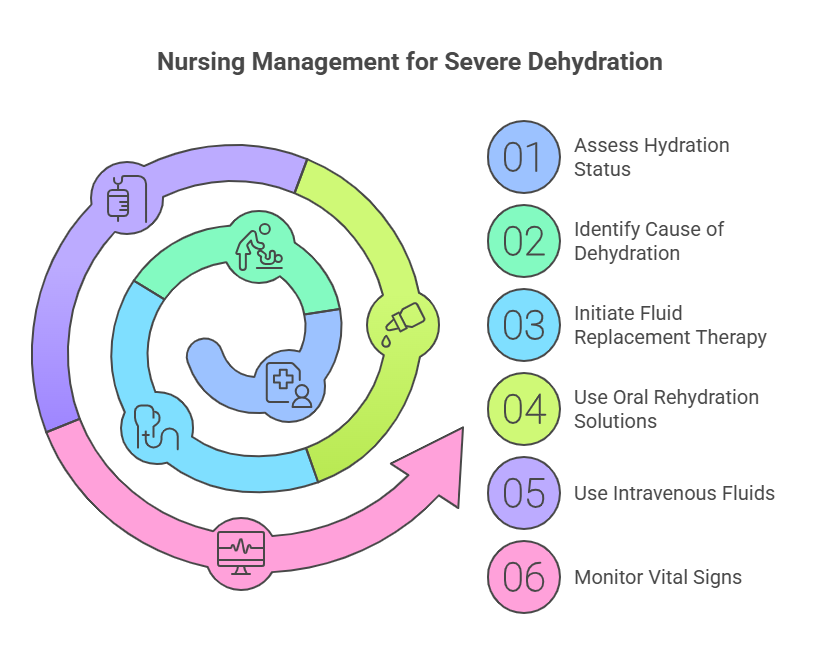
4.2.1. Dehydration
- Definition: Loss of body fluids, leading to electrolyte imbalance.
- Management: Oral rehydration solutions (ORS) for mild to moderate cases; IV
fluids for severe cases.

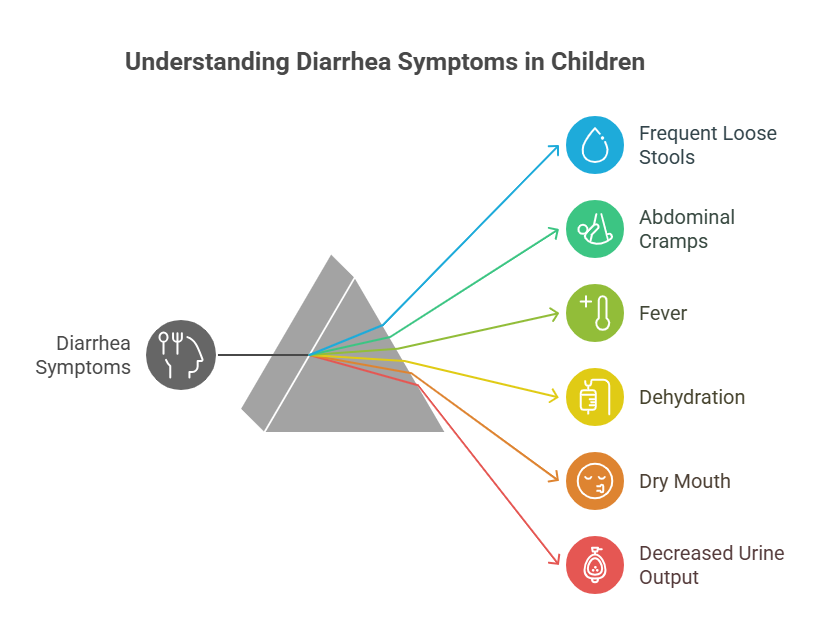
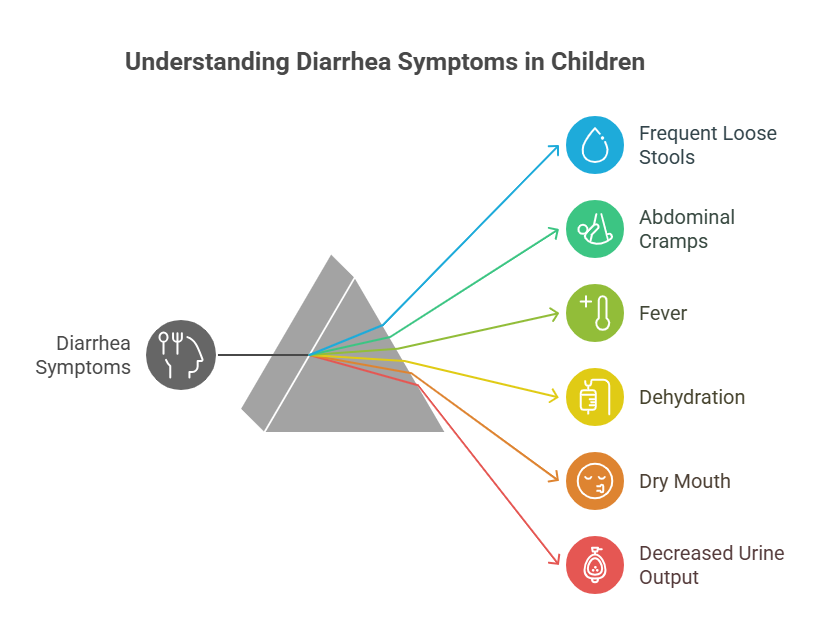
4.2.2. Diarrhea
- Key Points: Common in children; can lead to dehydration.
- Management: Focus on rehydration and dietary adjustments.
4.2.3. Dysentery
- Definition: Inflammation of the intestines, characterized by severe diarrhea
with blood. - Management: Antibiotics may be required; rehydration is essential.

4.2.4. Ear Problems
- Common Issues: Otitis media is prevalent in children.
- Management: Pain relief and antibiotics if bacterial infection is suspected.

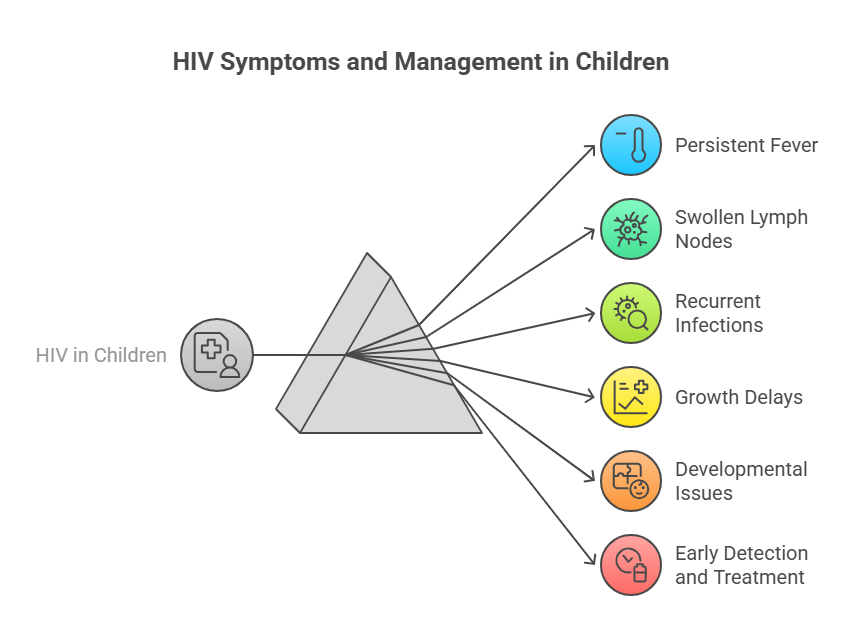
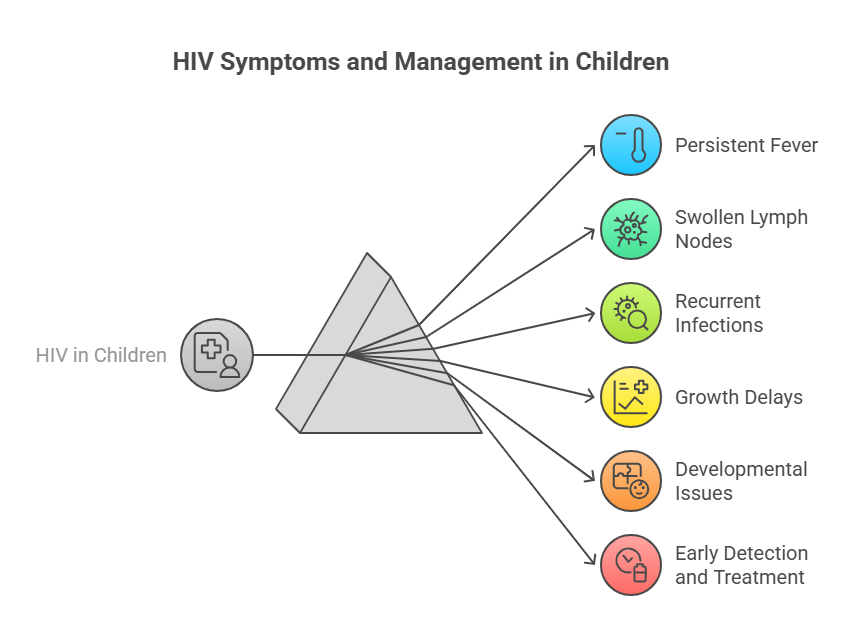
4.2.5. HIV
- Key Points: Early diagnosis and antiretroviral therapy are crucial.
- Management: Regular monitoring and supportive care.
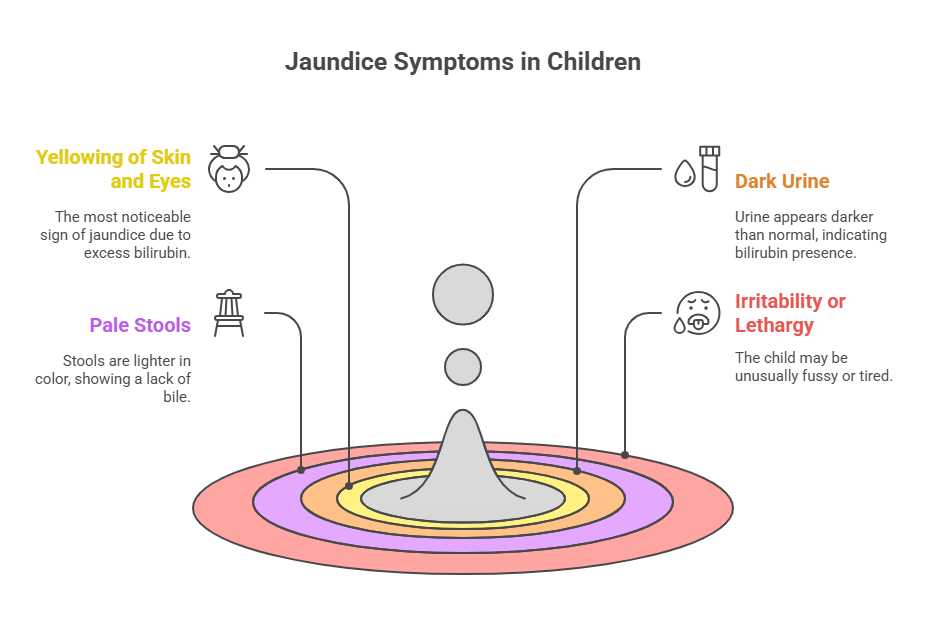
4.2.6. Jaundice
- Definition: Yellowing of the skin and eyes due to bilirubin accumulation.
- Management: Phototherapy for newborns; underlying causes must be identified.
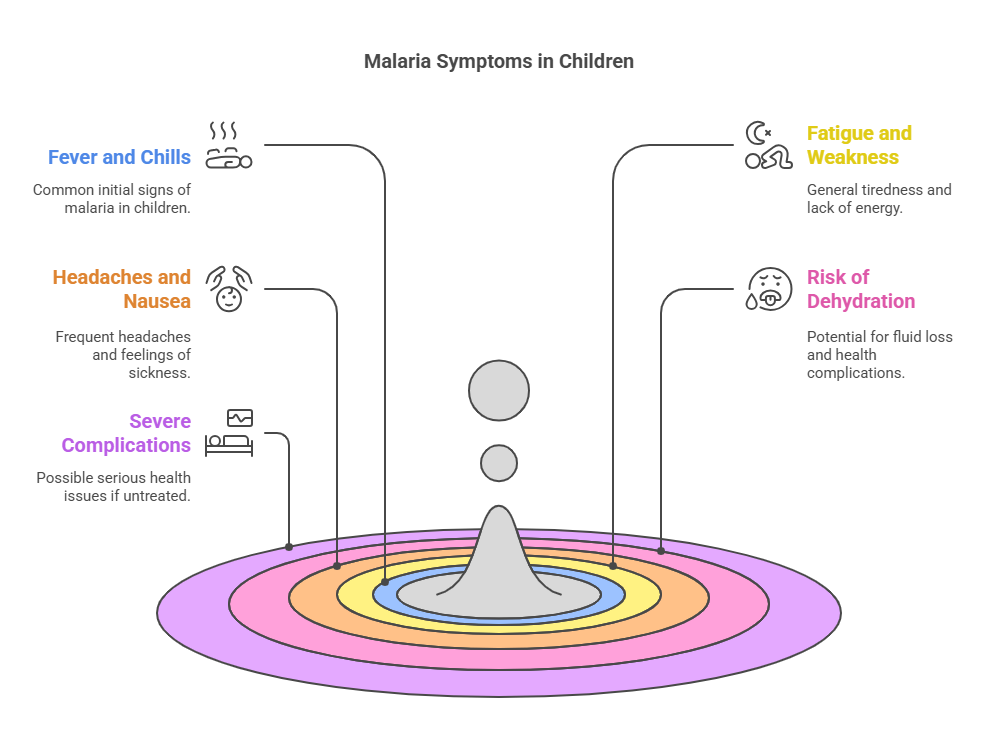
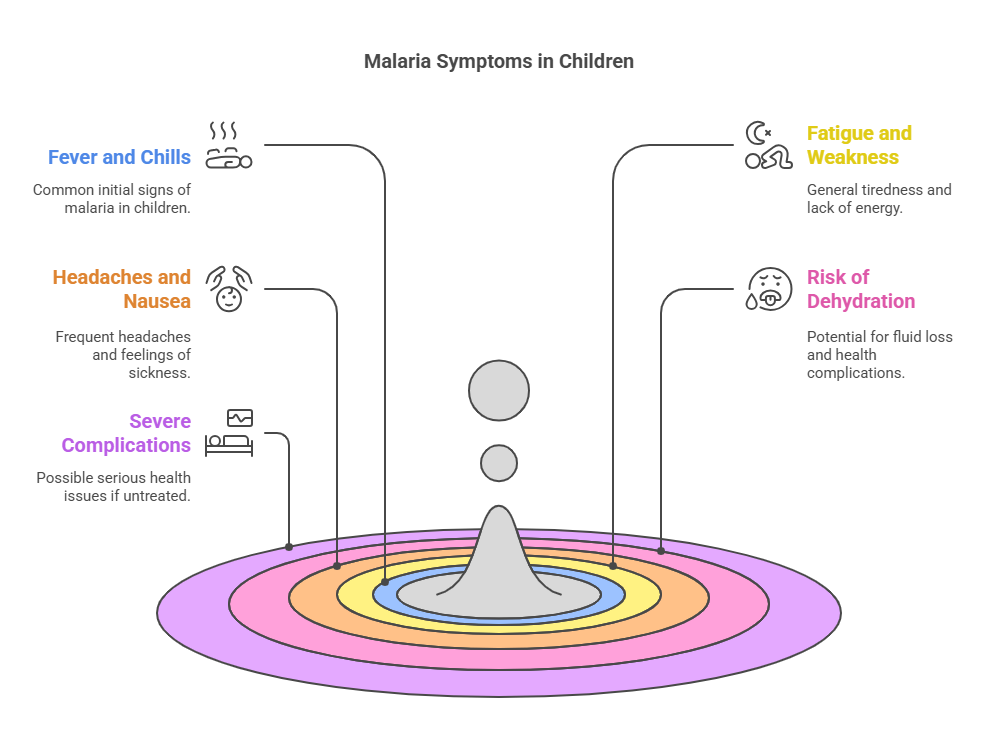
4.2.7. Malaria
- Key Points: Preventable and treatable; endemic in certain regions.
- Management: Prompt diagnosis and treatment with antimalarial drugs.
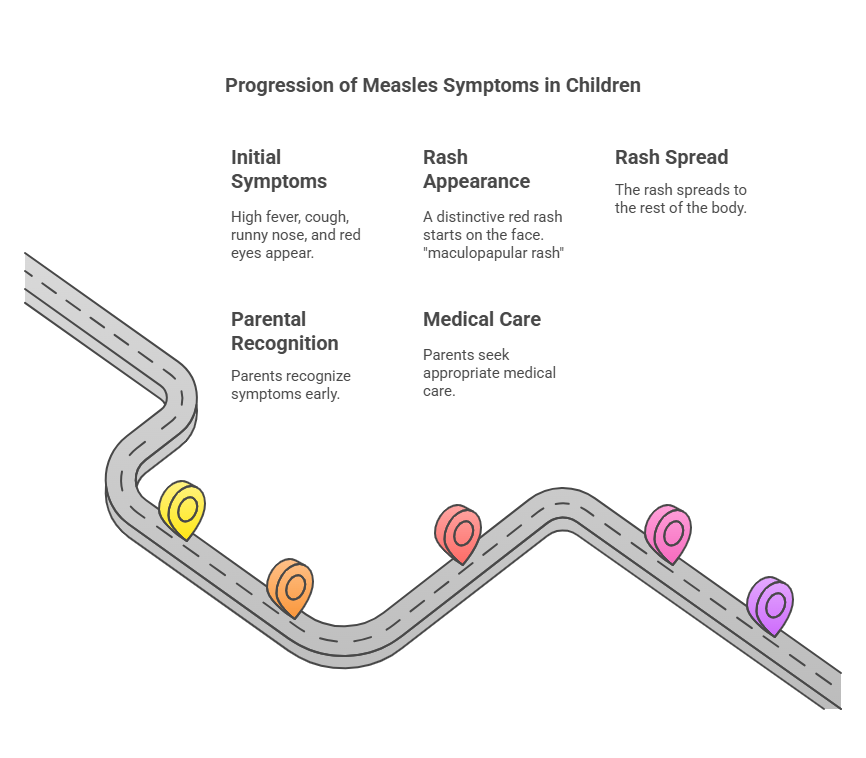
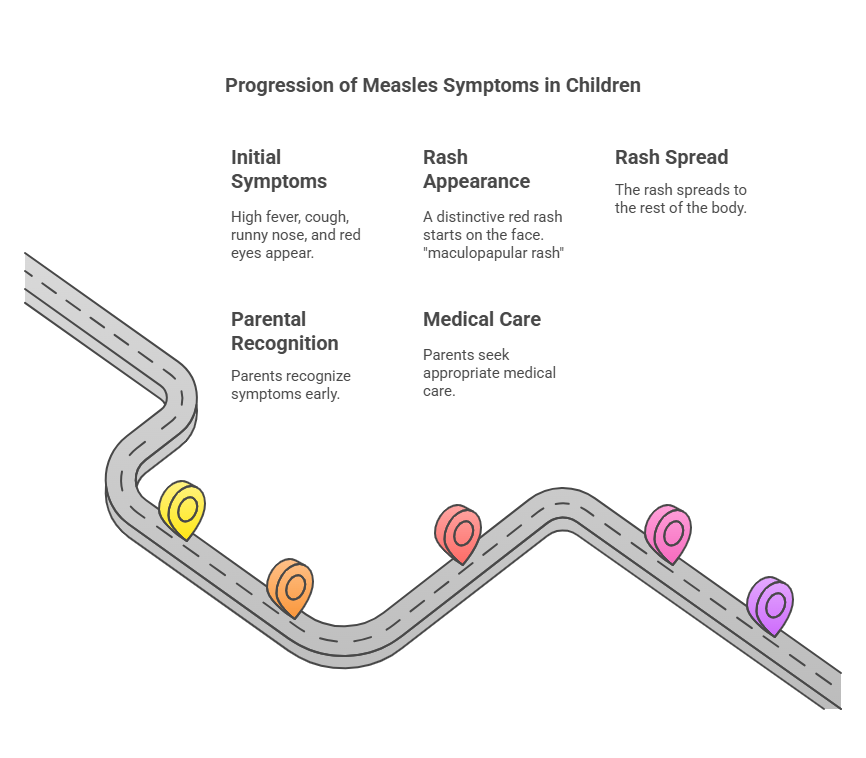
4.2.8. Measles
- Definition: Highly contagious viral infection, from 1 -2 days before onset
of symptoms up to 4 -5 days after the disappearance of rash. Incubation
period of 8 -12 days. - Management: Supportive care; vaccination is key for prevention.
- Transmission: Direct contact with infectious airborne droplet.
- Clinical Manifestation:
- 3 C’s of Measles:
C – ough C- onjunctiva C- oryza
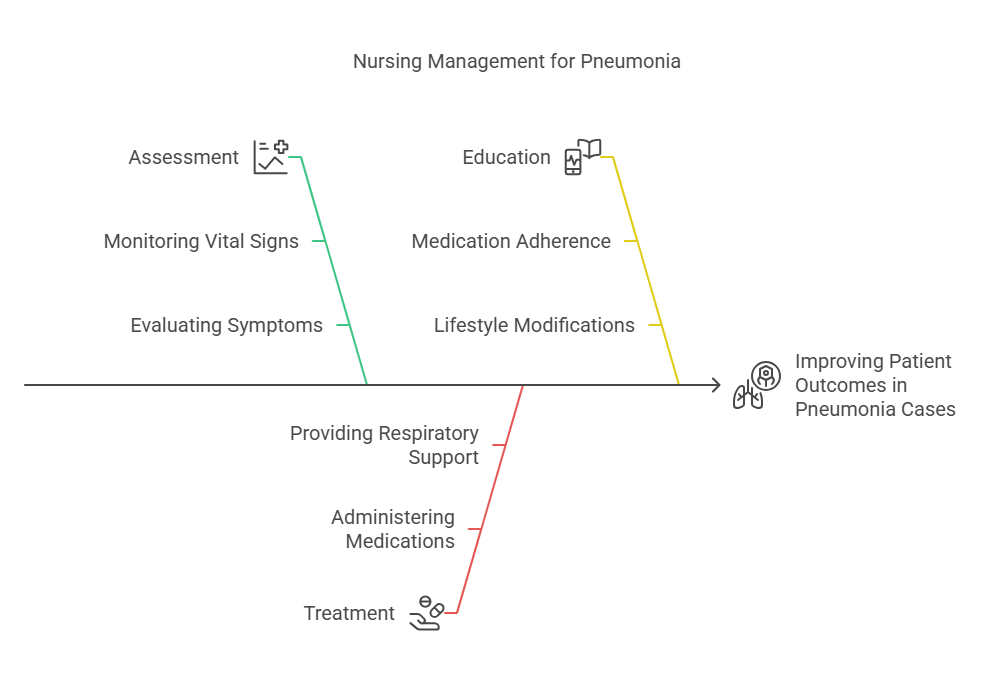
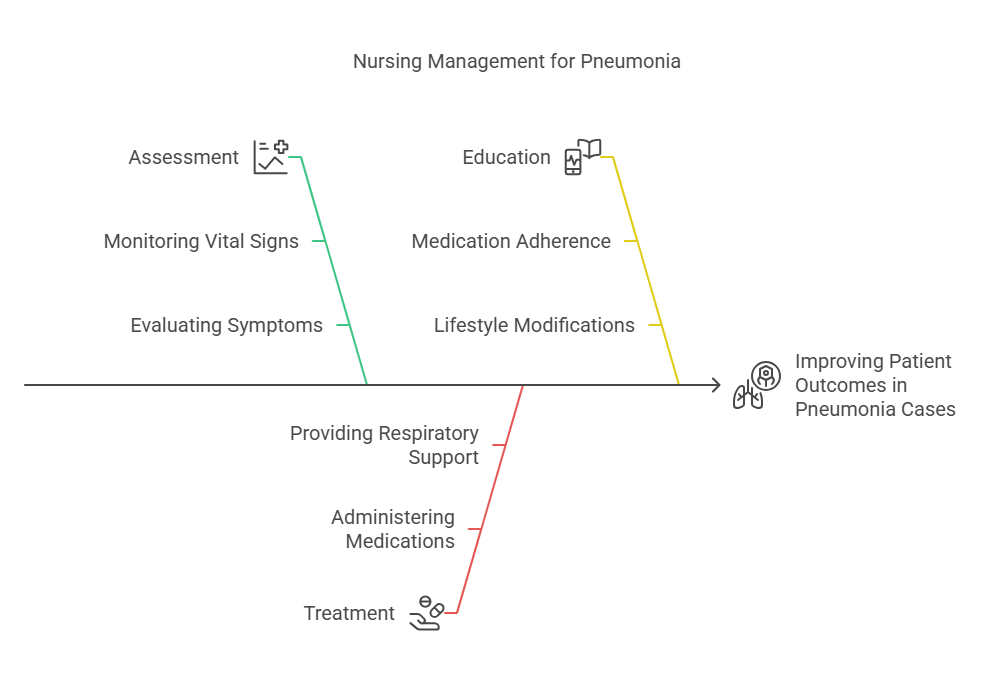
4.2.9. Pneumonia
- Key Points: Leading cause of morbidity and mortality in children.
- Clinical Manifestation: Elevated temperature, cough. Expectoration
of blood-tinged or purulent sputum, dyspnea, chest pain
- Management: Antibiotics for bacterial pneumonia; supportive care for viral
cases.
4.3. Danger Signs
4.3.1. Recognizing Life-Threatening Symptoms
- Key Symptoms: Difficulty breathing, lethargy, unresponsiveness.
4.3.2. Severe Dehydration
– Sleepy (Difficult to Awaken) – Sunken Eyes – Sip-less (unable to drink) – Skin
Turgor Very Poor or skin pinch goes back very slowly
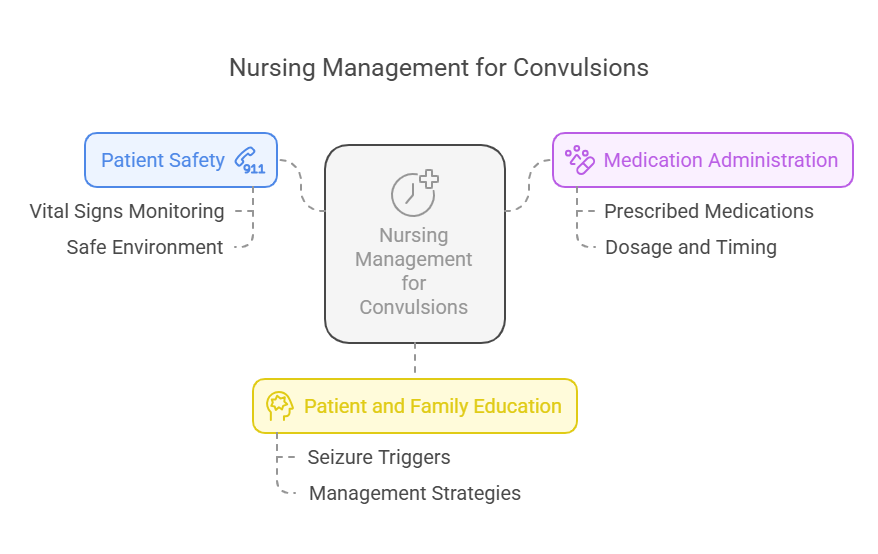
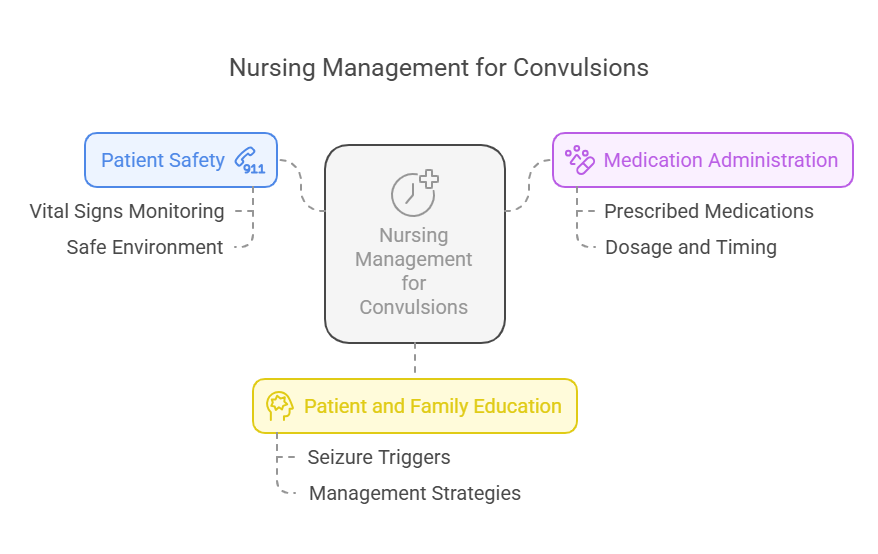
4.3.3. Convulsions
- Management: Immediate medical evaluation and treatment.
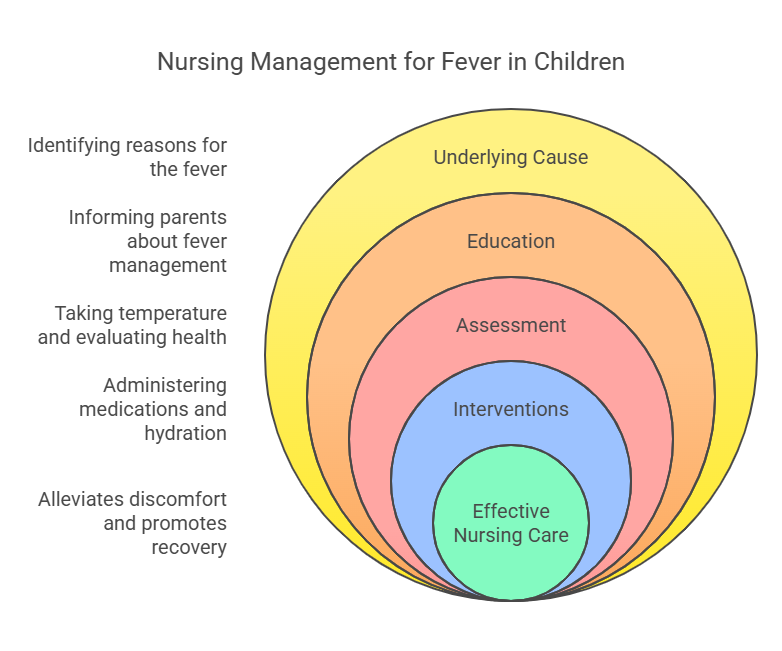
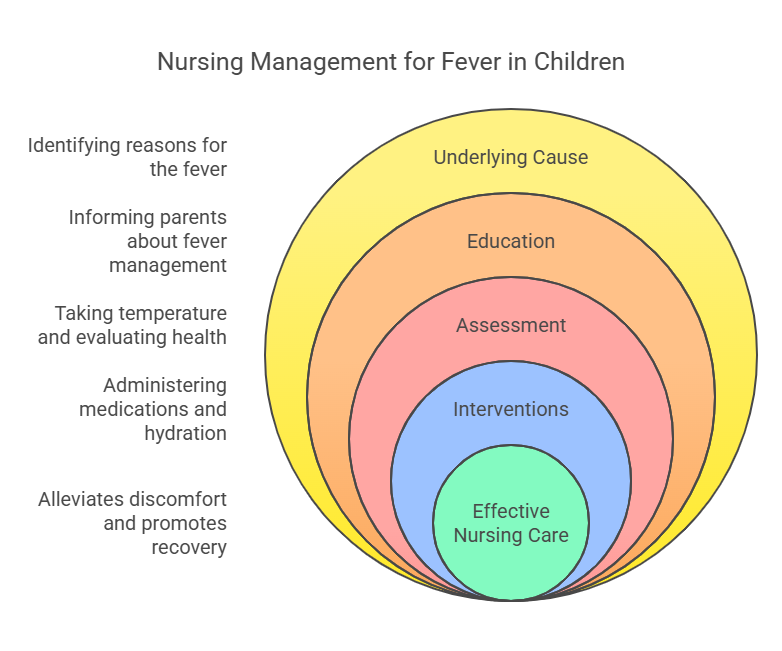
4.3.4. Fever in Children
- Key Points: High fever can indicate serious infection; requires prompt
assessment.
Relevance to the PNLE Exam
- Understanding IMCI is vital as it encompasses a significant portion of
pediatric nursing questions on the PNLE. - Focus on recognizing danger signs and managing common childhood illnesses,
as these are frequently tested.
Practice Questions
- Which of the following is a sign of severe dehydration in a child?
- A) Normal skin turgor
- B) Sunken eyes
- C) Increased appetite
- D) Clear urine
Correct Answer: B) Sunken eyes. Rationale: Sunken eyes are a classic sign of
severe dehydration.
- What is the first-line treatment for uncomplicated diarrhea in children?
- A) Antibiotics
- B) Oral rehydration solution
- C) Intravenous fluids
- D) Antidiarrheal medications
Correct Answer: B) Oral rehydration solution. Rationale: ORS is effective in
preventing dehydration due to diarrhea.
Quick Tips
- Mnemonic for Danger Signs: “”DASH”” – Difficulty breathing, Abnormal
lethargy, Severe dehydration, High fever. - Always assess hydration status in children presenting with diarrhea.
Take-Home Message
Mastering the Integrated Management of Childhood Illnesses is essential for
effective nursing practice and critical for success on the PNLE.
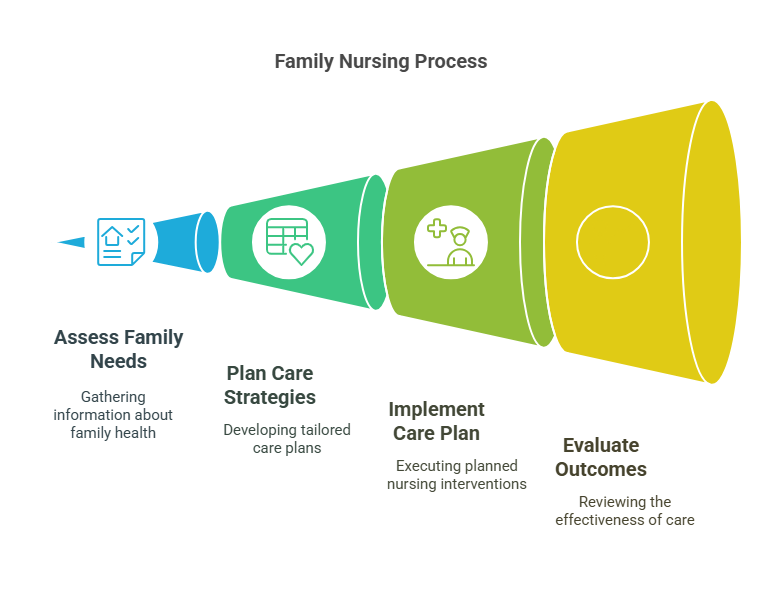
5. Family Nursing Process
General Introduction
This chapter focuses on the Family Nursing Process, a systematic approach to
providing care that considers the family unit as a whole. It encompasses
assessment, diagnosis, planning, implementation, and evaluation of nursing care
tailored to families, ensuring a comprehensive understanding of their health
dynamics. This guide is designed to assist Nursing Graduates in preparing for
the PNLE by emphasizing critical concepts relevant to family nursing.
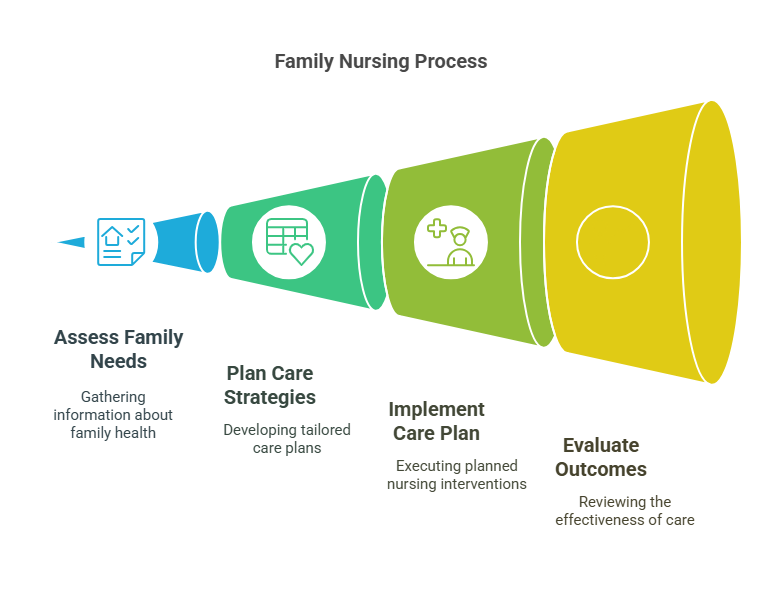
5.1. Family Health Assessment
Key Definitions
- Family Health Assessment: A comprehensive evaluation of the family’s health
status, dynamics, and needs. - Family Data Analysis: The process of interpreting data collected during the
assessment.
Key Principles
- Use of various tools to gather information about family structure, function,
and health. - Consideration of cultural, social, and economic factors affecting family
health.
5.1.1. Family Data Analysis
- Analyzing data to identify health patterns and risk factors within the
family.
5.1.2. Tools for Assessment
- Genograms: Visual representation of family relationships and medical
history. - Ecomaps: Diagram illustrating the family’s social environment and support
systems.
5.2. Family Nursing Diagnosis
- Identification of health issues within the family context.
- Formulation of nursing diagnoses based on assessment findings.
5.3. Formulating Family Nursing Care Plan
Key Definitions
- Family Nursing Care Plan: A structured plan that outlines nursing
interventions to address family health issues.
Key Principles
- Establishing clear, measurable goals and objectives for family health
improvement.
5.3.1. Establishing Goals and Objectives
- Goals should be specific, measurable, achievable, relevant, and time-bound
(SMART).
5.3.2. Intervention Strategies
- Tailored interventions addressing the unique needs of the family, including
education, support, and resources.
5.4. Implementing Family Care Plan
Key Definitions
- Implementation: The process of executing the nursing care plan.
Key Principles
- Coordination among healthcare providers to ensure comprehensive care.
5.4.1. Categories of Intervention
- Direct Care: Hands-on nursing interventions.
- Indirect Care: Activities that support the family indirectly, such as
referrals and advocacy.
5.5. Evaluation of Family Nursing Care
Key Definitions
- Evaluation: The process of determining the effectiveness of the nursing care
plan.
Key Principles
- Continuous assessment of outcomes to ensure goals are met.
5.5.1. Evaluation Process and Outcomes
- Use of feedback from family members to assess the impact of interventions
and modify the care plan as necessary.
Relevance to the PNLE Exam
- Family nursing concepts are frequently tested, particularly in scenarios
involving family dynamics and health assessments.
Practice Questions
- Which tool is used to visualize family relationships and medical history?
- A) Ecomap
- B) Genogram
- C) Care Plan
- D) Health Assessment
Correct Answer: B) Genogram Rationale: A genogram provides a visual
representation of family relationships and health history, essential for family
health assessments.
- What is the primary purpose of establishing goals in a family nursing care
plan?- A) To increase paperwork
- B) To ensure family involvement
- C) To provide a clear direction for interventions
- D) To limit nursing interventions
Correct Answer: C) To provide a clear direction for interventions Rationale:
Goals guide the nursing process and ensure that interventions are focused and
effective.
Common Misconceptions
- Misconception: Family nursing is only about individual patient care.
- Clarification: Family nursing considers the family as a unit, addressing
collective health needs rather than just individual concerns.
Quick Tips
- Remember the acronym SMART when setting goals: Specific, Measurable,
Achievable, Relevant, Time-bound.
Take-Home Message
The Family Nursing Process is essential for delivering holistic care that
addresses the unique health needs of families, ensuring effective assessment,
planning, implementation, and evaluation.